Dr. Jones (in blue) from Walter Reed and Dr. Goldbach-Mansky (in red) from the NIH welcoming all to the 1st Autoinflammation & Immune-dysregulation Symposium.
A National Center for Autoinflammatory Diseases Kick Off
The Autoinflammatory Alliance is proud and honored to have been involved in the collaboration, development, promotion, and to have provided financial support for the 1st Symposium of Autoinflammatory and Immune-Dysregulatory Diseases. The symposium was held at Walter Reed National Military Medical Center (WRNMMC) and was a collaboration between the National Institutes of Health (NIH) and WRNMMC, which are located across the street from each other. It was a great success! Researchers from various institutes at the NIH and WRNMMC, and from around the U.S. attended the symposium.
This symposium was more than just educational presentations; it’s main purpose was to usher in the official launch of a new national autoinflammatory center of excellence jointly run by experts from WRNMMC and the NIH. This collaboration is the first of its kind in the U.S. between the military and NIH, and it will help improve care, treatment, collaboration, and medical training so more patients can get the help they need. This is the start of a plan for a national network of autoinflammatory centers around the U.S, and for more collaboration and the development of consistent standards for diagnosis, treatment, and best practices for care. This is greatly needed, and having a central hub and support from the NIH and WRNMMC for this network will help significantly.
And now for the 1st Annual Autoinflammatory Symposium 2016 highlights!:
Over 16 speakers, that included patients and researchers, spoke about patient needs and the history, present, and future of autoinflammatory and immune system research. Directors and representatives from several WRNMMC departments and NIH institutes spoke of their resources that could be used for this new autoinflammatory center.
From every speaker there was a common theme—that research leads to treatment. We must know the causes (e.g., genetics, pathways) to get to treatment. And we must have follow-up studies after genetics are found.
Dr. Goldbach-Mansky and Dr. Oclay Jones – Welcome Note
Dr. Raphaela Goldbach-Mansky, M.D., M.H.S. of the NIH NIAID, and Chief of the Translational Autoinflammatory Disease Studies Unit and Dr. Oclay Jones, Chief pediatric rheumatologist with WRNNMC, were the founders of this symposium and the collaboration between WRNMMC and the NIH. They both welcomed attendees to the symposium that was to ignite an NIH/WRNNMC collaborative autoinflammatory center of excellence.
Goals of the center include:
- Providing primary care to autoinflammatory patients, under joint research protocols for military and civilian patients.
- Be a place for a second opinion visits, and a way to get other specialists and testing done for patients at either WRNMMC or the NIH.
- Telemedicine appointments with local doctors for consultation and continued care at home will be developed.
- Education and outreach for doctors and patients, and expanded training for young investigators and rheumatology fellows are also planned.
Dr. Jones mentioned that 50% of children covered by the Department of Defense (DOD) live in a state with only one or no civilian pediatric rheumatologist, which makes caring for periodic fever syndromes very challenging for these families. This center will able to better help those families, plus civilian patients that are in need of care at this center, or that are already in NIH clinical trials that need some care and testing that is available at WRNMMC.
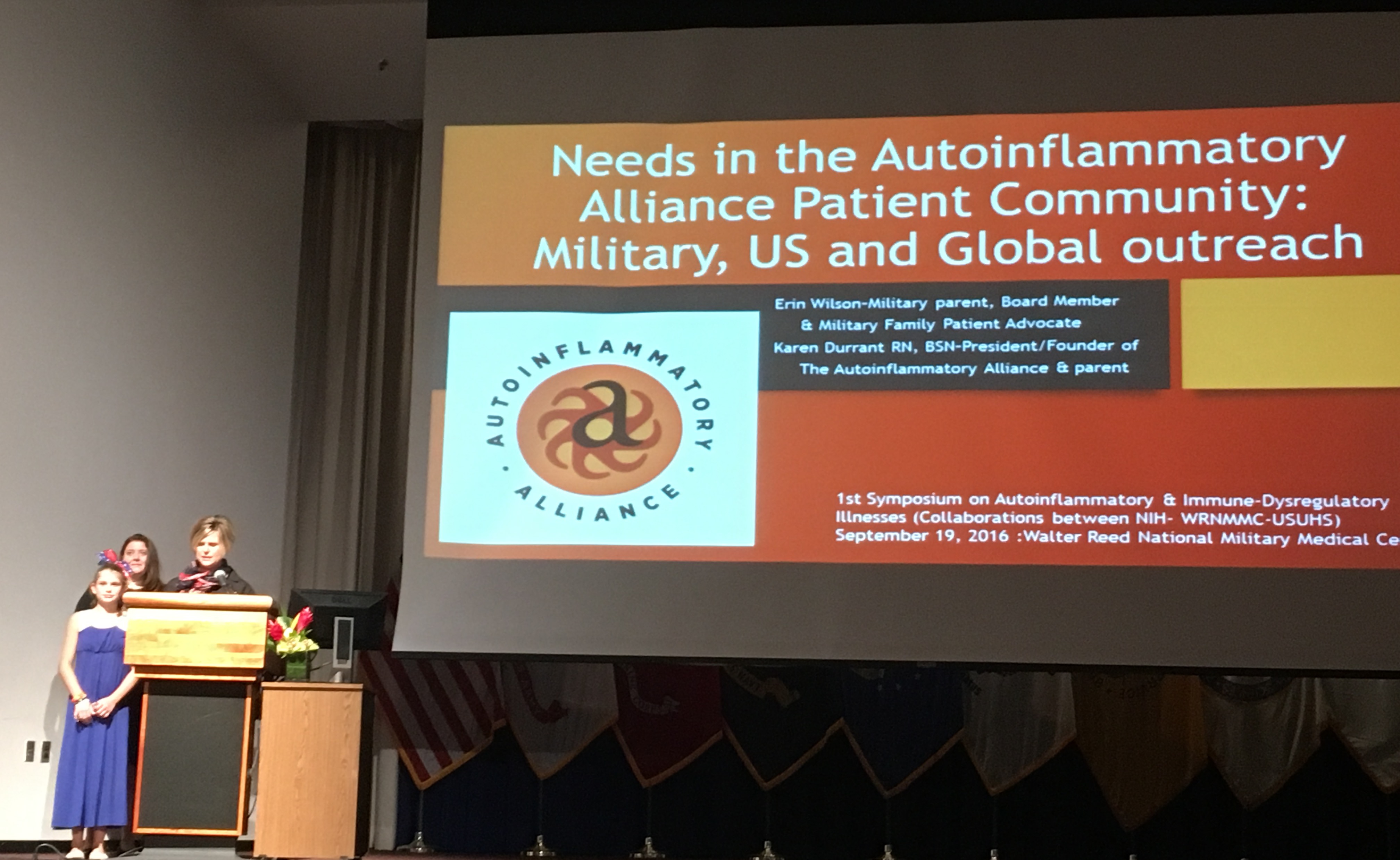
Autoinflammatory Alliance President Karen Durrant and Board Member Erin Wilson (speaking) discuss the needs of autoinflammatory patients and challenges they face getting medical care.
The Autoinflammatory Alliance’s Karen Durrant and Erin Wilson – Needs in the Community
Karen Durrant, R.N., B.S.N., and Erin Wilson from the Autoinflammatory Alliance spoke about autoinflammatory patient needs. Erin Wilson spoke of the struggles with getting a diagnosis and treatment for her daughter with HIDS (hyper-IgD syndrome, a Mevalonate Kinase Deficiency (MKD) disease) as a military family, which comes with its own unique challenges.
Karen Durrant emphasized early and correct diagnosis, along with the correct treatment is essential to help patients have the best outcomes, and a healthier life. Many of the known autoinflammatory diseases have some treatments that can help to control inflammation, but more research is needed, and understanding of disease pathways. Even with the current treatments that are available, some of these diseases need more specialized and targeted treatments that have not been developed yet. There are challenges for patients in the United States, and globally with getting a diagnosis, and even genetic testing, along with access to the right treatments. Having a center of excellence dedicated to these diseases, helping to develop best practices for care and treatment, and education for doctors is essential. Thus, there is a need for a National Center for Autoinflammatory Diseases that combines NIH and WRNNMC expertise, research, and resources for patients, and training and collaboration with outside doctors.
Dr. Dan Kastner – The Revolution of Genetics and Genomics in Defining Immune Dysregulation, from Monogenic to Polygenic Diseases
Dr. Daniel Kastner, M.D., Ph.D., and Scientific Director of the NHGRI at the NIH, and one of the world’s experts on autoinflammatory diseases, gave a fascinating overview of the history of using DNA to diagnose and ultimately treat patients with these syndromes. Dr. Kastner was the researcher that came up with the term “autoinflammatory.” His enthusiasm and passion for DNA is contagious. He makes genetic testing and biologic pathways very exciting. If you have never watched one of his talks, you can do so here and here.
He went over the history of learning about variants in DNA that could cause diseases in the 1970s, to what is known today about the genetics. In the 1970s researchers first discovered that variants in DNA could cause disease, but the first 20 years of genetic research was very slow due to lack of technology, and the difficulty and cost of sequencing DNA. Today DNA sequencing is faster and more inexpensive. However, interpreting the data from current sequencing studies is the challenge, and takes a lot of time. In the past 5 years, Dr Kastner and his colleagues have made many discoveries of new genes, including many newly classified autoinflammatory diseases, which has led to better treatment for these patients.
Dr. Kastner first became interested in periodic fever syndromes when an Familial Mediterranean Fever (FMF) patient peaked his interest in the genetic pathways of such diseases. In 1985, he started his pursuit to find the FMF gene and in 1997 Dr. Kastner and his team discovered the FMF gene which they named MEFV (Mediterranean Fever). It took 12 years to find that first periodic fever syndrome gene, but today because of technology, the cost of DNA sequencing has dramatically dropped, and the speed of such testing has dramatically increased, and new diseases are being classified more quickly.
Dr. Kastner used the discovery of the DADA2 gene (deficiency of adenosine deaminase 2, aka fever with early onset stroke) as an example of how research in genetic testing has led to effective treatments for patients. DADA2 causes recurrent fevers, severe livedo reticularis, and early-onset lacunar strokes. It is treated with TNF antagonist biological medications. Currently there are 27 patients with DADA2 in the NIH and Israel studies. Before genetics were understood for this condition those 27 patients had 44 strokes combined in 1064 patient months. (Click here to learn more about the DADA2 study.) Once researchers found the genetic cause, understanding the pathway quickly followed which led to trying anti-TNF medications. Since this discovery, there have been 0 strokes in 323 patient months with this cohort of DADA2 patients.
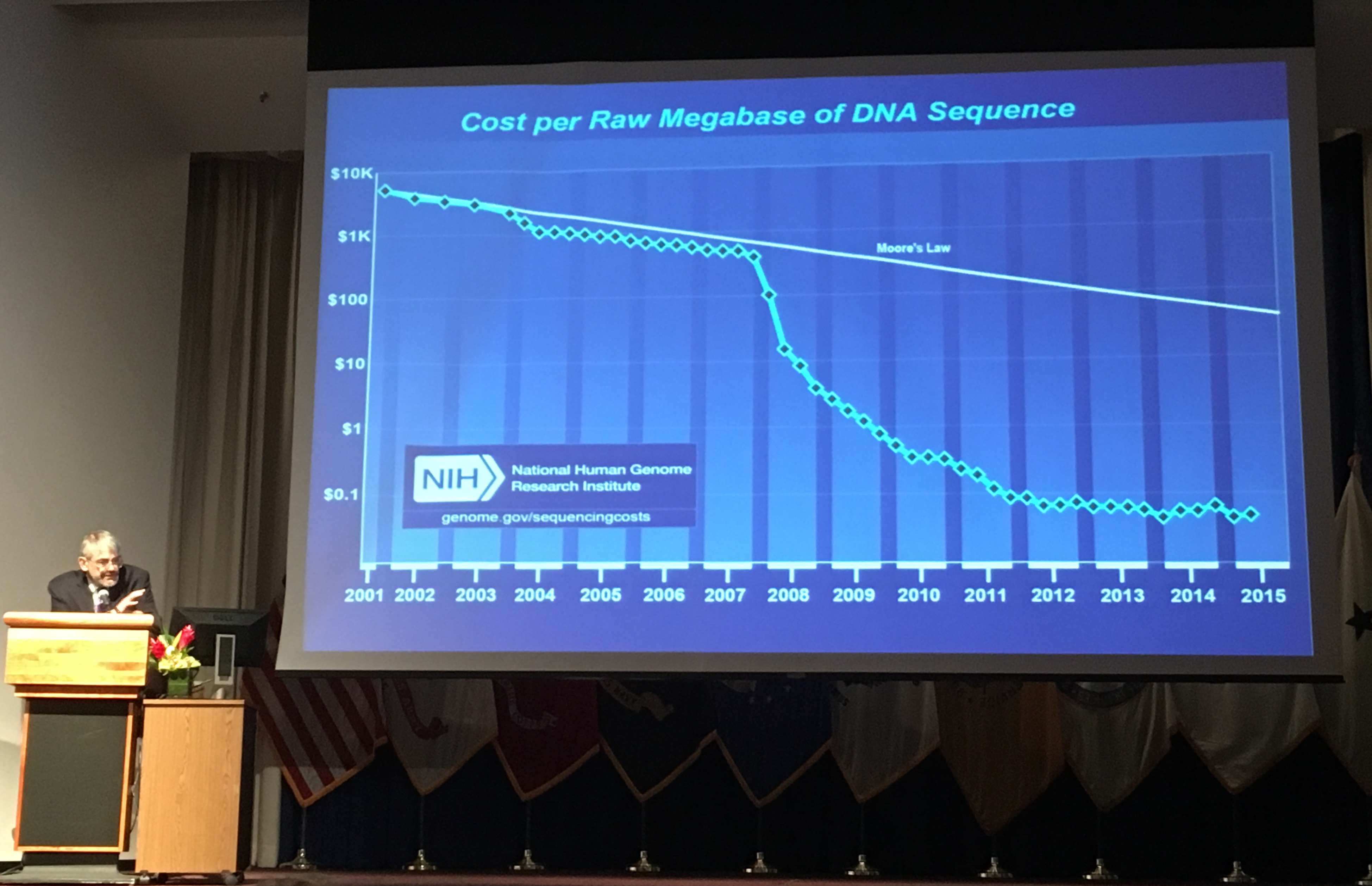
Here Dr. Kastner of the NIH shows how dramatically the cost of genetic testing has dropped over the last 10 years.
Dr. Goldbach-Mansky – Challenges of Treating Patients with Rare Immune-dysregulatory Diseases—The Needs to Form Networks and to Work with the Pharmaceutical Industry
Dr. Goldbach-Mansky (NIH-NIAID), an expert in autoinflammatory diseases, also emphasized the need for research in genetics and pathways of these diseases in order to develop effective treatments and stated that,
“Access to genetics should be part of a diagnostic work up for any child with autoinflammatory symptoms.”
She discussed the process of how the development of target therapies starts with genetics. She further talked about challenges they will face and overcome when developing an autoinflammatory disease network of centers. Also mentioned was the need for collaboration with pharmaceutical companies to development new and better treatment options.
Challenges for an Autoinflammatory Disease Network:
- Implementation of genetic testing for all patients, that includes WES/WGS for patients with negative genetics for known syndromes and somatic mutation testing.
- Developing a standard immune work up that includes cytokine analyses and gene expression in blood and organs.
- Improving treatment access and effectiveness that includes developing treatment guidelines and more clinical trials.
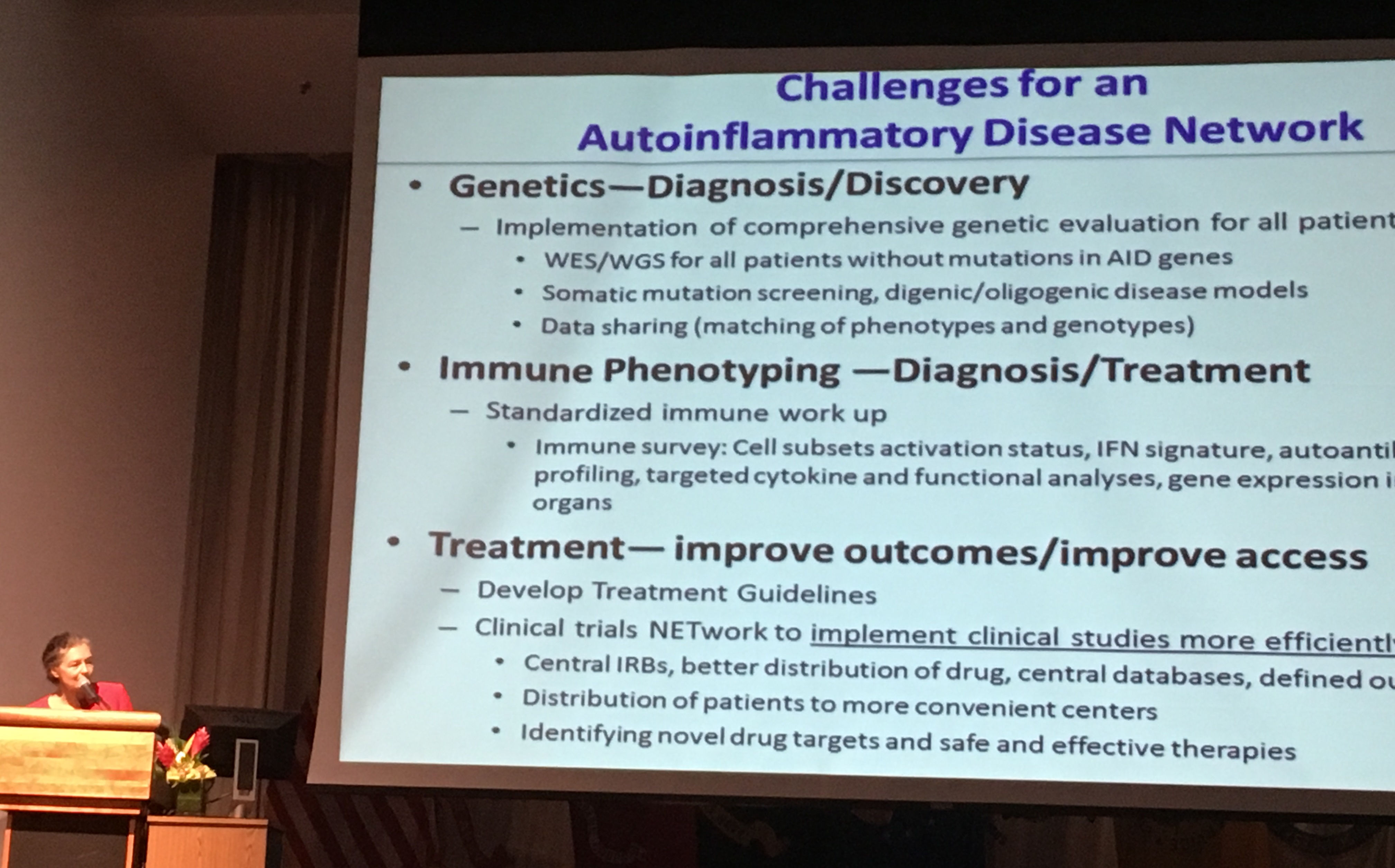
Dr. Goldbach-Mansky of the NIH discusses the challenges of developing an autoinflammatory disease network of clinical centers. These are challenges the NIH and WRNNMC are ready to take on.
Other Speakers
Several WRNNMC departments and experts, such as from pathology, pediatric, infectious disease, and medical technology, described their resources available that could be used by the Autoinflammatory Center and how such resources fit into a precision medicine model of health care.
Navy Commander Margaret Read, the executive assistant for the deputy chief for readiness and health of the Navy Bureau of Medicine and Surgery gave a wonderful speech about systemic JIA and macrophage activation syndrome (MAS), and it’s impact on her child’s life, and how care under Dr. Jones and the staff at WRNMMC saved his life. It was very touching. Her son, who was in attendance with her, is under better disease control with the right care and treatment from specialists. Her story is featured here on the WRNMMC newsroom, and it is a very touching testimonial about the challenges of SJIA and MAS.
For more highlights from WRNMMC researchers, and a summary of many of the speakers, read page 4-5 of the WRNMMC Department of Research Programs October 2016 edition of the Military Medical Research Newsletter
2016 Autoinflammatory Symposium Military Family Roundtable Discussion
At the end of the symposium speakers and attendees broke up into roundtable discussion groups. The representatives from the Autoinflammatory Alliance attended the Military Family Roundtable, where military families discussed what difficulties and help they’ve had navigating the military medical system with a family member who has a chronic illness. Below are highlights of that discussion.
- Difficulty with getting necessary testing. One problem is some facilities can only use certain labs which limits test availability.
- Many families are not told about services and programs available to them that can help navigate the medical system, such as the Exceptional Family Member Program (EFMP) that helps to assist and support military families with special medical and educational needs.
- They would like help with educating doctors on their rare disease. Every time they move, they have to explain everything to a new doctor.
- There is high turnover of pediatricians in the military system. So in addition to the families’ moves and deployments, their military pediatricians also go on new deployments, or are reassigned. This makes continuity of care with a primary doctor very difficult.
- Medical records are not all in one location within the military system, and some have civilian medical records that are not connected to the military medical system. Patients must make sure to maintain their own copies of all their records to give to the doctors when needed.
- Case managers can set up combined appointments. Military families can apply for a case manager. However, some families said that case management slows things down. Others say it speeds things up. It seems to depend on the location of the family in the military medical system.
- Having a serious medical diagnosis in the family impacts the families greatly, and limits a military career path. Whether it’s a mild or severe, both are treated the same for assignments, and the family will only be assigned to be wtihin a set distance near medical services.
- Different branches of the military have different systems.
- Everyone agreed on the wonderful care that WRNMMC provides and in particular how fabulous Dr. Jones is.
- Families expressed a great need for a more streamlined process to get into WRNMMC.
- “It’s doable.” – That was the message from the military representatives at the roundtable.
We are looking forward to a full day symposium for the next conference that is being planned for September 2017 and for the launch of the joint center for autoinflammatory diseases between the NIH and WRNMMC that will open in 2017. It was a pleasure to be a part of this project, that has been a goal that started with a discussion with Dr. Jones and Dr. Goldbach-Mansky a few years ago. We are so happy that they too saw this need, and worked so hard to make this possible. The Autoinflammatory Alliance will be actively involved in supporting this symposium, autoinflammatory research center, and other research projects for years to come.
Please click here to donate now to support our efforts for education and research so we can support more projects like this! Thanks to all that have supported us, and helped to make this important symposium and collaboration between WRNMMC and the NIH possible.
More Reading
- NIH: Rare Autoinflammatory Diseaess Research: Saving Lives, Giving Hope to Families
- IEEE Pulse: The Precise–and Wild–Genomic Revolution: Genomics Provides Novel Treatments for Disease and is Opening New Frontiers for Precision Medicine
- WRNMMC Department of Research Programs October 2016, volume 9 edition of the Military Medical Research Newsletter