 Updated 6/11/21
Updated 6/11/21
Autoinflammatory diseases, also commonly known as periodic fever syndromes, are systemic inflammatory diseases caused by malfunctions of the innate immune system. Most autoinflammatory diseases are genetic chronic lifelong diseases that typically have the first symptoms start in childhood. However, due to the complex range of symptoms and their rarity, patients with these conditions may not get diagnosed or effective treatment until they are adults. And in some cases, the first symptoms don’t appear until adulthood.
In addition, some patients may be diagnosed with autoinflammatory disease symptoms as a child, but the cause may not have been classified, or determined yet, and these patients are still seeking a diagnosis, often into adulthood. Experts on autoinflammatory diseases estimate that up to 2/3 of their patient population has a systemic undifferentiated autoinflammatory syndrome , so it is important to consider systemic autoinflammatory diseases as a possible diagnosis in a patient that has the following symptoms, even if the genetic cause has not yet been identified or symptoms started in adulthood.
Typical Autoinflammatory Symptoms and Lab Results
Symptoms vary between the different autoinflammatory syndromes, but there are some common symptoms that many share:

Severe abdominal pain is a common symptom of some fever syndromes, such as FMF and HIDS. Patients may have a history of being misdiagnosed with appendicitis and/or food poisoning.
- recurrent fevers (without an infectious cause; may occur every month or randomly)
- rashes
- joint pain and/or arthritis
- mouth ulcers
- gastrointestinal symptoms including vomiting and/or diarrhea
- stomach or chest pain
- red eyes (non-infectious conjunctivitis)–some may even get uveitis and/ or iritis (inflammation in the eyes)
Many autoinflammatory diseases have similar lab results including:
- high inflammatory markers (CRP, ESR, SAA)
- high WBC
- most have negative ANA and other autoantibody tests
Some autoinflammatory diseases cause chronic inflammation that can affect any organ system in the body over time. This includes:
- sensorineural hearing loss
- enlarged liver and/or spleen
- bone involvement
- secondary amyloidosis
- aseptic meningitis (either during flares or chronically, depending on the autoinflammatory disease)
- Gastrointestinal inflammation, ulcers, or perforations
Depending on the syndrome, many will have flares of symptoms that can last for a few days to several weeks, while some will have continuous inflammatory symptoms. Between flares, some patients may be asymptomatic with normal lab values. But for those with mild to moderate chronic symptoms, even when they do not have a fever, they may have elevated inflammatory markers, other abnormal labs and/or symptoms related to chronic inflammation.
It’s important to note that the above list represents the most common presentation of many autoinflammatory diseases, but there are some who do not have typical symptoms.
It is essential that physicians consider autoinflammatory diseases as a possible diagnosis when they are presented with a patient who has recurrent fevers or other signs of systemic inflammation, especially since childhood, along with other symptoms such as rash and/or arthritis. With genetic testing and resources to compare symptoms, doctors should be able to diagnose, and treat more patients.
Many Adults are Still Misdiagnosed and Suffering
Some adult specialists may see patients who were not properly treated for their disease throughout their life who have developed the most severe complications associated with their disease. This is because many patients come into adulthood without an accurate diagnosis and/or correct treatment due diagnostic challenges. Some of these challenges include these being rare diseases with a lack of information on these diseases in medical school, many being newly discovered diseases, and some patients not presenting as a textbook case making diagnosis difficult.
Most of the autoinflammatory diseases have had their genetic cause discovered in the past 15-20 years. In addition, thanks to genetic testing and collaboration by experts worldwide, many newly classified autoinflammatory diseases have been identified in the past 15 years or less, so many patients that were previously undiagnosed may get help now.
Also, these conditions may be easily missed in childhood and thought to be just recurring, typical childhood illnesses. With common symptoms, such as fever, the symptoms may not raise suspicion early on. Over time the symptoms and affects of systemic, chronic inflammation may be more apparent. Some conditions may go into remission for months to years at a time or the symptoms may change throughout life, which may make it difficult to notice a regular pattern for symptoms.
Some patients may have symptoms that are more pronounced, or debilitating as adults, but others may have their symptoms reduced, or present differently in adulthood. Some patients may not have the typical presentation for their disease, such has not having fevers, but can still develop severe complications such as amyloidosis. For example, there is a form of adult-onset familial Mediterranean fever (FMF) that the first noted symptom is amyloidosis in various organs of the body.
In Cryopyrin-associated Periodic Syndrome: CAPS Seen from Adulthood Dr. Isabelle Kone-Paut writes, in regards to CAPS that, “The diagnostic delay is deleterious to patients compromising their quality of life and exposing them to neurosensory complications and renal failure by secondary amyloidosis.”
Adult Patients Need Compassion from Medical Professionals
When patients come into an adult specialty practice after years of being undiagnosed, and untreated, or misdiagnosed and without proper treatment, they may have more damage and complications from their disease that needs expert care. In addition, many patients that reach adulthood without a diagnosis have endured great stigmas and challenges emotionally, and the affects of chronic illness can affect their ability to work, or obtain their full potential in education or a career. A number of adult patients may stop seeing doctors, as they have “given up” on doctors ever finding out what they have, or how to treat it, or have been told too commonly that “it’s all in your head.” Their loved ones are often the ones that push them to try one more time to get help for their disease. So, it is essential to consider the needs of the patient on all levels, and address any unmet psychosocial concerns in a compassionate way with these patients.

Genetic testing can help diagnose autoinflammatory diseases. Click here for information on genetic testing.
Genetic Testing
Genetic testing for known autoinflammatory diseases can help to accurately diagnose patients and help guide treatment. Many patients report they were first misdiagnosed before getting genetic testing. Reported prior misdiagnoses in autoinflammatory patients include: Cancer, allergies, Sjogren’s, leukemia, lupus, allergies, fibromyalgia, Crohn’s disease, immunodeficiency, infections, and appendicitis.
In the U.S. there are now several periodic fever panel genetic tests available that test for most all known fever syndromes at one time and at very reasonable cost.
Other Diagnostic Tools
Other tools that can help with diagnosing patients who are suspected of having an autoinflammatory disease include:
Autoinflammatory Search –The Systemic Autoinflammatory Diseases (SAID) Database – This database is based on the Comparison Chart of Systemic Autoinflammatory Diseases that was reated and edited by Autoinflammatory Alliance President Karen Durrant, RN BSN as a co-author on the chart and database with many leading experts on autoinflammatory diseases,. Here you can search for symptoms and lab results to get a list of autoinflammatory conditions to consider, and find many helpful resources and links to medical publications for each disease. This comparative chart has become a highly respected and important diagnostic tool for doctors and patients around the world, and this new search database is the most current, updated and easy to use method for learning about autoinflammatory diseases available at the moment.
Eurofever Classification Criteria – This quiz gives a risk score that a patient may have TRAPS, HIDS, FMF, or CAPS based on specific symptoms a patient has.
Also it’s essential that patients keep an accurate symptom log as the pattern of symptoms greatly helps with diagnosis. Click here for more symptom logs used by autoinflammatory patients.
Adult-onset Autoinflammatory Diseases as an Atypical Presentation
It is most common for these syndromes to start in childhood, however there are documented patients with adult-onset symptoms with what are typically considered infant or childhood-onset fever syndromes. It’s important not to discount autoinflammatory diseases as a possibility just because the patient’s symptoms did not start in childhood.
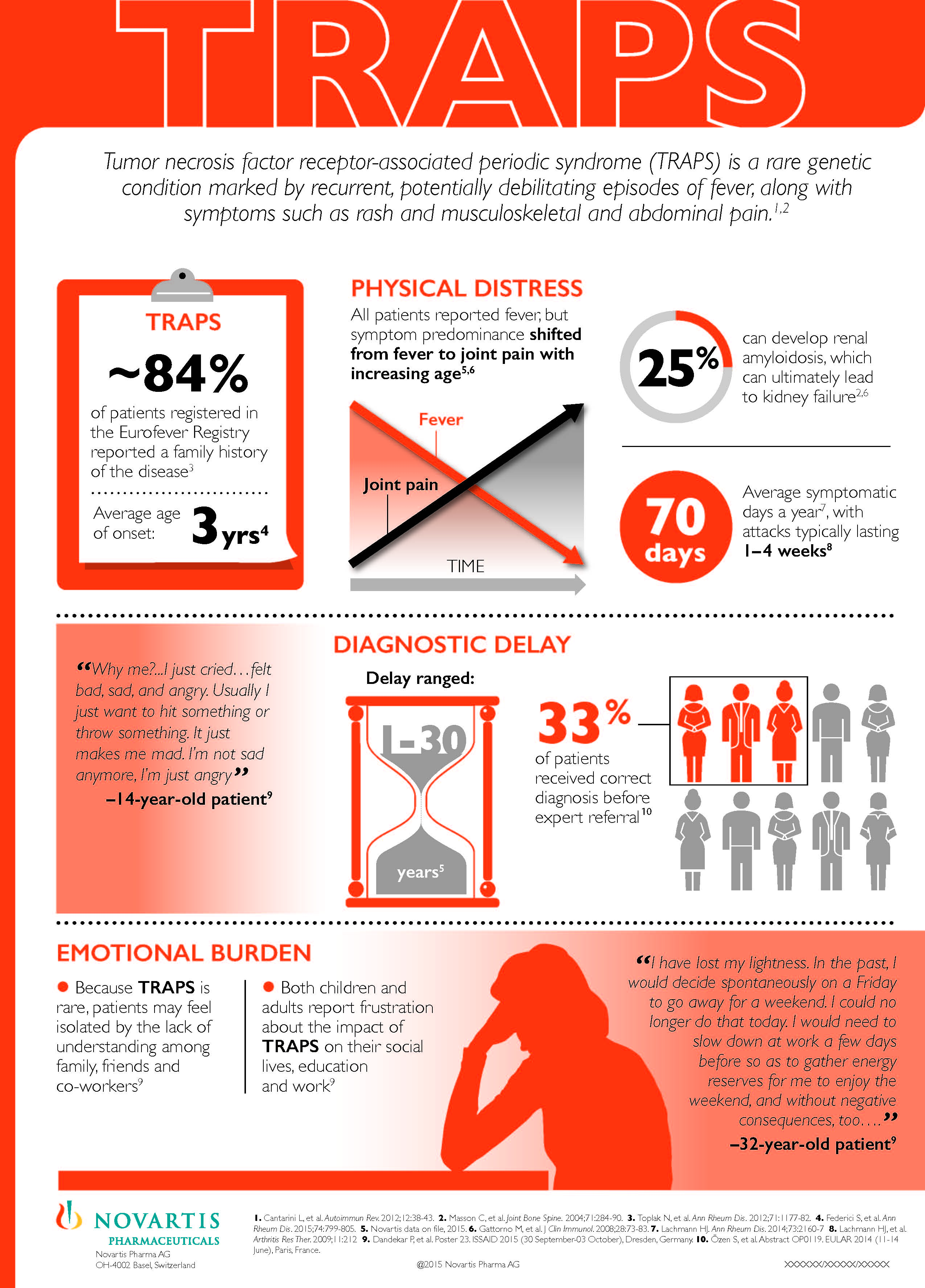
For example, patients with FMF (familiar Mediterranean fever), HIDS (hyperimmunoglobulinemia D with periodic fever syndrome), TRAPS (tumor necrosis factor (TNF)-associated periodic syndrome), CRMO (chronic recurrent multifocal osteomyelitis), DITRA (deficiency of interleukin-36 receptor antagonist), and CAPS (cryopyrin-associated periodic syndromes, including: FCAS, Muckle-Wells and NOMID/CINCA) typically develop symptoms in early childhood, but all have reported some adult-onset cases. In CAPS, patients that do not present with symptoms until adulthood are often found to have either a variant genetic mutation for CAPS, or they may have somatic mosaicism, which occurs when the genetic mutation that causes disease is not found in all cells. Somatic mosaicism can be missed on standard genetic testing. In the past, 40% of patients with clinical symptoms of CAPS did not have their genetic mutation identified on standard testing, but when the newer, specialized tests were done, over 99% of those patients had their mutation found, and most had somatic mosiaicsm.
Dr. Lachmann et al reported in a 2014 study published in the Annals of Rheumatic Diseases that 22% of study participants had adult-onset TRAPS.
Adult-onset presentations of these diseases may have an atypical clinical presentation than childhood-onset. According to the authors of Clinical and genetic characterization of the autoinflammatory diseases diagnosed in an adult reference center published in Autoimmunity Reviews in 2015, “Compared to children, adult patients with AID in our series presented more frequently with non-severe manifestations and none of them developed amyloidosis during follow-up. Adult patients also carried higher proportion of low-penetrance mutations or polymorphisms and all genetic variants were presented in heterozygosis or as heterozygous compounds.”
A few Classified Autoinflammatory Diseases Start in Adulthood
A few autoinflammatory diseases are different in that they rarely or never start in childhood and most patients will not develop symptoms until they are adults. Some autoinflammatory diseases known to more commonly have symptoms start in adults include: Adult-onset Still’s disease (age 16 to 35 most commonly), Behçet’s (20s to 30s), and Schnitzler’s (most cases start in middle age at over 35 to 50 years old).
Fertility, Pregnancy, and Breastfeeding
Adult patients may have concerns about becoming pregnant and having a healthy pregnancy. Many patients with an autoinflammatory disease do have successful healthy pregnancies. However, some fever syndromes are associated with increased infertility and certain risks during pregnancy. In some cases, it’s been noted that having good treatment and control of the disease symptoms and inflammation reduces those risks.
Because of possible risks and complications before and during pregnancy, both the rheumatologist and obstetrician need to closely monitor autoinflammatory patients during pregnancy.
Fertility
There are very few studies regarding fertility and autoinflammatory diseases, but likely each syndrome affects fertility differently. The authors of the study Muckle-Wells syndrome and male hypofertility: a case series concluded that, “MWS may be associated with subfertility and infertility in male patients.” When left untreated, FMF is known to cause infertility in both men and women. The authors of the study No appreciable decrease in fertility in Behçet’s syndrome determined that infertility was not increased among Behcet’s patients.

Many autoinflammatory patients have healthy pregnancies, however both the rheumatologist and obstetrician need to closely monitor patients during pregnancy.
Pregnancy
In some, but not all, autoinflammatory diseases, pregnancy does present some higher risks and complications for both the mom and baby. Patients with adult-onset Still’s disease have an increased risk for preterm birth and intrauterine growth retardation. FMF, when not treated increases the risk of miscarriage, premature birth, low birth weight in babies, and infertility in both men and women. Patients with Behçet’s disease have an increased risk for vascular complications, however one study noted that “neonatal outcomes were not negatively influenced by Behçets Disease.”
Having an autoinflammatory disease, however, does not guarantee that there will be problems with pregnancy. Some moms report that they felt the best they ever felt while pregnant because their disease went into remission during their pregnancy. The Autoinflammation website notes that in HIDS, “During pregnancy, attacks can disappear, but delivery can trigger an attack.”
At this time, any decision to use any medication during pregnancy or breastfeeding to treat an autoinflammatory disease in the mother is a strictly off-label, experimental use (not approved by the FDA or EMEA) for these medications.
The choice to use any medication should be made by the patient and their doctor.
It can be difficult making decisions about treatment during pregnancy. Some are fortunate to have fewer symptoms or even complete remission during pregnancy. For those who need treatment throughout pregnancy, there is limited information on the safety of commonly used medications for these diseases. Most biologics have not been studied for safety during pregnancy in autoinflammatory patients, however there are a few small studies where anakinra was used either daily or intermittently in pregnant autoinflammatory patients. These patients were better able to control their disease symptoms with treatment and most had otherwise healthy pregnancies and babies. Adverse events that did occur, such as renal agenesis, were not conclusively related to the use of anakinra. In some cases, the adverse event was a known risk associated with the mother’s autoinflammatory disease.
The authors of Brief Report: Anakinra Use During Pregnancy in Patients With Cryopyrin-Associated Periodic Syndromes concluded that continuing treatment of CAPS women during pregnancy with anakinra, “provided significant, persistent symptom relief while continuing to prevent the long-term sequelae of CAPS.”
Colchicine, the most effective treatment for FMF, has been used in pregnant women, in various reports for over 30 years. However, colchicine is listed as a class C medication by the FDA so it is important to discuss the use of medication during pregnancy with a physician.
A number of medical journal reports have found that in patients with FMF that have taken colchicine during pregnancy, that there were no significant negative effects in the infants, and the pregnant FMF patients also had a good outcome. According to the National Amyloidosis Centre in regard to FMF patients, “The chances of successful pregnancy outcome are actually better in patients who are careful to take their colchicine.”
This 2010 study found that colchicine had no impact on pregnancy and reported that, “Treatment with colchicine during pregnancy in patients with FMF is beneficial in controlling the disease while not affecting the outcome of the pregnancy.”
We have more studies on autoinflammatory treatments, pregnancy, and breastfeeding here.
Breastfeeding
Colchicine has had a limited number of studies of use while breastfeeding. Colchicine does appear in human breast milk, at the same level as found in the mother’s plasma. There have been no signs of serious complications in infants that breastfed from mothers that were taking colchicine in various reports, but it is important to review the research findings, and discuss the options with a doctor. According to the drug information for colchicine on drugs.com:
“Limited information suggests that exclusively breastfed infants receive less than 10 percent of the maternal weight-adjusted dose. While there are no published reports of adverse effects in breast-feeding infants of mothers taking colchicine, colchicine can affect gastrointestinal cell renewal and permeability. The manufacturer warns that caution should be exercised when administering colchicine to breastfeeding women and their infants should be observed for adverse effects.”
According to Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk, Il-1ra (anakinra is an Il-1ra), is naturally secreted in higher amounts than in the blood into breastmilk in healthy individuals. It is not currently known what the levels of anakinra are in human breast milk, or if drinking Il-1RA from the milk is, or is not absorbed in the intestines. So it is important for patients to discuss the pros and cons or breastfeeding and the unknowns of anakinra use during breastfeeding with their doctor. This same guidebook states,
“Because of the presence of native Il-1ra in milk, there appears to be no risk to a nursing infant from maternal administration of anakinra.”
Many Treated Patients Are Now Living Longer and Healthier Lives–But Still Have a Lot of Unknowns
In the last 30 years, research has led to great advancements in the diagnosis and treatment of patients with autoinflammatory diseases. Genetic testing has led to a better understanding of the causes and mechanisms leading to inflammation in patients with autoinflammatory syndromes. Biologic medications that target the intracellular drivers of autoinflammation have helped many patients to have improved overall health, less flares or symptoms of their autoinflammatory disease, and reduced chronic inflammation.
Once fatal conditions, such as NOMID (neonatal-onset multisystem autoinflammatory disease) and DIRA (deficiency of interleukin-Iβ receptor antagonist), now have a better prognosis with these targeted treatments, especially if the patient is diagnosed and started on treatment early in life. Before targeted biologic treatments were available, 20% of patients with NOMID, the most severe form of CAPS (cryopyrin-associated periodic syndromes), did not survive into adulthood, and 100% of patients with DIRA died in early childhood, or infancy. Now these patients are living longer, and much healthier lives.
In the past, it was uncommon for many patients with the most severe autoinflammatory diseases to reach adulthood, so most adult rheumatologists or other physicians that only care for adult patients may not have encountered some of these rare, severe diseases, but these are lifelong conditions. Some of the less severe patients may go for years or decades without a diagnosis, and may present with symptoms that they have been dealing with for their entire life to an adult rheumatologist. So it is essential that these specialists consider autoinflammatory diseases when presented with a case that features many of the symptoms listed at the beginning of this article, especially if the patient has recurrent fevers, and other symptoms such as rashes.
With patients that have started treatment for their autoinflammatory disease in early childhood, and have had their symptoms well-controlled with their medications, an adult rheumatologist may not see the severity of chronic damage, or many of the “classic” symptoms, because treatments may have prevented some or all of the complications typically associated with their condition. An extensive health history can help to identify the patient’s symptoms, and the extent that the disease has affected their health and quality of life.
For some of these conditions, such as DIRA, that if untreated is always fatal in early childhood, it’s unknown what health challenges and complications the adults may face. It is hopeful that more and more patients will be living longer and healthier lives. But their medical future is still uncertain, as there is little known about the health of adults with some of these these severe autoinflammatory diseases.
For all adult autoinflammaotry patients, there is a great need for more awareness of these syndromes by adult specialty physicians that may encounter autoinflammatory patients in their practice.
References
- RareConnect: TRAPS Infographic
- PubMed.gov: Familial Mediterranean Fever With Complete Symptomatic Remission During Pregnancy
- PubMed.gov: A retrospective survey of patients’ journey before the diagnosis of mevalonate kinase deficiency
- PubMed.gov: The novel S59P mutation in the TNFRSF1A gene identified in an adult onset TNF receptor associated periodic syndrome (TRAPS) constitutively activates NF-κB pathway
- PubMed.gov: Clinical and genetic characterization of the autoinflammatory diseases diagnosed in an adult reference center
- Reumatismo: Childhood versus adult-onset autoinflammatory disorders: myths and truths intertwined
- PubMed.gov: Caution Should be Used in the Recognition of Adult-Onset Autoinflammatory Disorders: Facts or Fiction
- Autoinflammatory Alliance: NOMID/CINCA
- PubMed.gov: Cryopyrine-associated periodic syndrome: CAPS seen from adulthood
- PubMed.gov: The phenotype of TNF receptor-associated autoinflammatory syndrome (TRAPS) at presentation: a series of 158 cases from the Eurofever/EUROTRAPS international registry
- PubMed.gov: Brief Report: Cryopyrin-Associated Periodic Syndrome Caused by a Myeloid-Restricted Somatic NLRP3 Mutation
- PubMed.gov: The expanding spectrum of low-penetrance TNFRSF1A gene variants in adults presenting with recurrent inflammatory attacks: clinical manifestations and long-term follow-up.
- PubMed.gov: Clinical and genetic characterization of the autoinflammatory diseases diagnosed in an adult reference center
- PubMed.gov: No appreciable decrease in fertility in Behçet’s syndrome
- Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk
- PubMed.gov: Hyper-IgD syndrome and pregnancy
- PubMed.gov: Successful outcome of two pregnancies in patients with adult-onset Still’s disease treated with IL-1 receptor antagonist (anakinra)
- Wiley Online Library: Brief Report: Anakinra Use During Pregnancy in Patients With Cryopyrin-Associated Periodic Syndromes
- Pediatric Rheumatology: ANTI IL-1 therapies and pregnancy outcome
- BMJ.com: A patient’s wish: anakinra in pregnancy
- PubMed.gov: Adult-onsetl Still’s disease and pregnancy: about ten cases and review of the literature
- PubMed.gov: Behcet disease and pregnancy
- PubMed.gov: Retrospective evaluation of pregnancy outcomes in women with familial Mediterranean fever
- Amyloidosis.org: Colchicine in Pregnancy
- PubMed.gov: Muckle-Wells syndrome and male hypofertility: a case series
- PubMed.gov: Pregnancy outcomes in women with familial Mediterranean fever receiving colchicine: is amniocentesis justified?
*Adult fever photo by CandyBox Images
* Stomach pain photo by Yulia
* Pregnant photo by Bayu Aditya/Flickr



I have had frequent fevers that fluctuate from 97.6 which is normal for me, to 106. In one day, since August 2016. Sometimes with flu like symptoms, without body aches or headaches. My Dr. cannot figure out what the causes are. She gives me antibiotics that seem to work temporarily, but the fevers return. I’m 63 and healthy, my last physical was a week ago and my Dr. said most 30 year oldso would love to be this healthy. But I don’t feel healthy. I have frequent bouts of vertigo and loss of appetite for no apparent reason. Can you help me? I’m ready to give up.sincerely, Suzanne
Hello Suzanne,
I’m sorry you are suffering like this. It sounds like your doctor needs to consider autoinflammatory/periodic fever syndromes, but because these are rare many doctors are not familiar with them. Below are some links with information to share with your doctor. Also, please feel free to join our Facebook group Autoinflammatory Diseases-Rare But Not Alone! – https://www.facebook.com/groups/nomidalliance/
This goes over tests that doctors run to start with if someone is showing symptoms of a fever syndrome. These can also help to determine if autoimmune or an immune deficiency need to be considered as well. – http://saidsupport.org/child-keeps-getting-fevers/
This covers the genetic testing available that’s helpful in diagnosing one of these syndromes – http://saidsupport.org/patient-resources/finding-a-diagnosis/
And finally, this is the autoinflammatory database – go over it with all your doctors and discuss symptoms and anything else from it that stand out to you – http://www.autoinflammatory-search.org/
I hope this helps and you can get some answers and hopefully a treatment soon.
Jennifer
Dear Suzanne,
I would suggest having your doctor refer you to an infectious diseases doctor, and a rheumatologist if needed. Sorry you are suffering.
Karen
Hello
My 19year old son was diagnosed with pfd last year after suffering since early childhood. He’s recently lost his job because of absences and I just wondered how other people manage to hold down a job. Thanks
Dawn
Hello Dawn,
I’m sorry to hear his PFS is affecting him greatly. There are support groups he can join to get in touch with others who have the same condition and can offer support and advice for this.
This link lists some of those groups – http://saidsupport.org/patient-resources/support-groups/
Jennifer
Hello, I’am 58 years old .I have had once a month headaches since at least 1997, aches and pains always. After reading all this got me thinking I have been told I have fibromyalgia all the arthritis Sisters and brothers LOL!! I seem to take spurts feel great then feel like I got run over by a truck as a child I remember having pains in my right side ,Mainly when I danced .I would drink Milk and it went away . . I do not know if I have this but I have what I call my Hormonal Headache stiff joints. Thanks for any advise in advance
Hi Cat,
I’m sorry to hear about the symptoms you have. This post goes over steps to take and what to talk to the doctor about if you think you may have a fever syndrome – http://saidsupport.org/child-keeps-getting-fevers/
Jennifer
I’m suffering from fevers Drs are dismissing me help
Hi Lisa,
I’m sorry to hear you are suffering. This has information to learn more about fever syndromes and with what to talk to the doctors about. http://saidsupport.org/where-to-start/
Also we have a Facebook group that can be of more help to you – https://www.facebook.com/groups/nomidalliance/
Jennifer