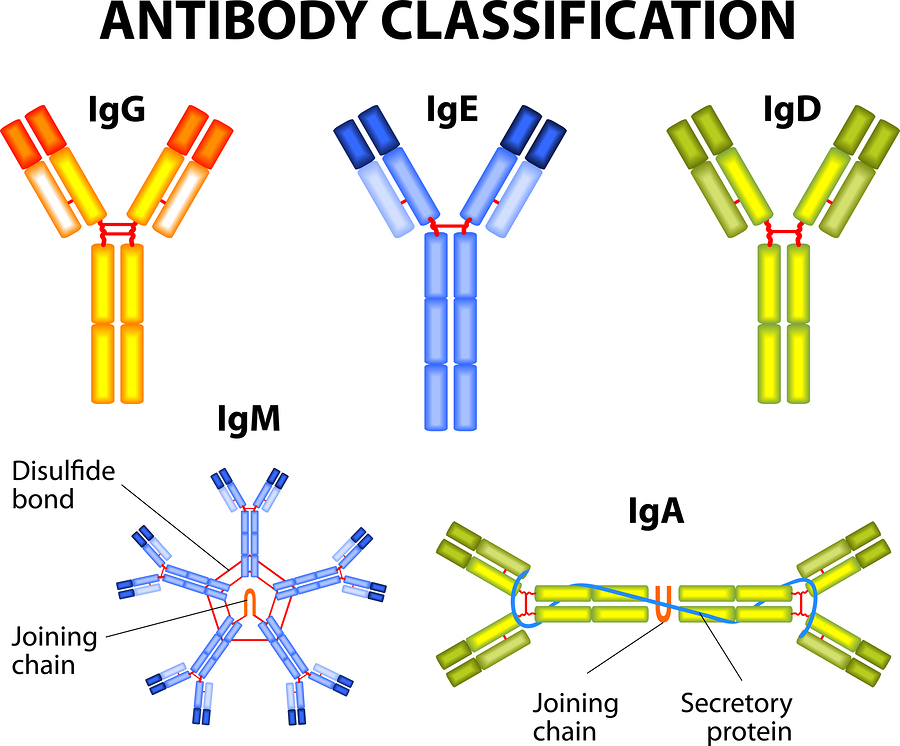
“Recent research shows that IgD is an important immunomodulator that orchestrates an ancestral surveillance system at the interface between immunity and inflammation.” 1 Photo by designua/Bigstockphoto.com
In 1984, Dr. Jos van der Meer published a study describing a newly recognized periodic fever syndrome. All six patients in this study had similar symptoms of periodic fevers with other inflammatory symptoms. They also all had elevated immunoglobulin D. This led to naming this new fever syndrome, hyperimmunoglobulinamia D and periodic fever syndrome, or HIDS for short. This study led to a better diagnosis for many because now a test for elevated IgD could be performed to help confirm a diagnosis of HIDS. But advancements in genetic testing has shown that elevated IgD is not diagnostic to HIDS.
In 1999, the gene responsible for HIDS was found. HIDS and MA (mevalonate aciduria) are caused by mutations in the mevalonate kinase gene (MVK), giving rise to the new classification for these conditions–mevalonate kinase deficiencies (MKD). This discovery led to great advances in understanding HIDS and MA.
By using genetic testing as part of the diagnosis and research into HIDS, studies now show that elevated IgD levels are not the best diagnostic method for HIDS. About 20% of patients with HIDS, confirmed by genetic testing, do not have elevated IgD. Children with HIDS under age three almost never have elevated IgD. Plus some patients with other fever syndromes, such as PFAPA, TRAPS, and FMF can also have elevated IgD. Some with undifferentiated autoinflammatory disease may also have elevated IgD levels.
In addition, according to Toro et al in this study, elevated or high IgD levels can be found in other conditions, including, “multiple myeloma, Hodgkin disease, cigarette smoking, pregnancy, immunodeficiency syndromes, and recurrent infections.”
While it’s true that most with mevalonate kinase deficiencies (MKD) have elevated or high IgD, and it’s less common or rarely elevated in other fever syndromes, basing a diagnosis on IgD results becomes problematic when evaluating individual patients, especially considering that PFAPA, TRAPS, and FMF also have symptoms that are similar to HIDS.
Below is a collection of studies and quotations from the research related to IgD in periodic fever syndromes.
PFAPA (Periodic Fevers with Aphthous Stomatitis, Pharyngitis, and Adenitis)
Elevated immunoglobulin D levels in children with PFAPA syndrome – In this study, PFAPA patients that did not have mutations in the MVK gene (HIDS/MA) and met the clinical diagnosis for PFAPA had high IgD in the range of about 300 to 350 U/I. Elevated IgD was found in all the PFAPA patients in this study. “Raised IgD levels may represent a non-specific epiphenomenon, which frequently accompanies PFAPA syndrome as well as MKD. Because of the overlapping clinical and laboratory features, genetic testing of the MVK gene is indicated to differentiate these two conditions.”
HIDS and MA
Autoinflammatory diseases in childhood – “Increased plasma levels of IgD (>100 UI/ml) during fever episodes and in basal conditions have been considered in the past as a hallmark of the disease. However, the specificity of this finding is low. The polyclonal elevation of serum IgD is found mostly in patients older than 3 years, but this is not exclusive for MKD, while in 20% of patients there is no increase of serum IgD.”
MVK mutations and associated clinical features in Italian patients affected with autoinflammatory disorders and recurrent fever – “IgD plasma level was found increased or minimally increased (>100 UI/ml) in only 10/15 patients, five of whom showed also increased IgA levels (>400 mg/dl)… Two cases…showed a remarkable increase of only IgA, a condition already reported in MKD and, finally, in three patients both IgD and IgA levels resulted in the normal range.”
“This latter definition does not comply any longer with this disease, because of the increasing evidences of patients showing normal IgD levels, as confirmed by the finding of normal or minimally elevated serum IgD in nearly half (seven out of 15) of the MKD patients reported here. Consequently, IgD level cannot be considered a sensitive marker for clinical MKD diagnosis.”
Hyperimmunoglobulinemia D and periodic fever syndrome (HIDS) in a child with normal serum IgD, but increased serum IgA concentration – “This report describes a boy with hyperimmunoglobulinemia D and periodic fever syndrome (HIDS). The serum IgD level was normal, but the serum IgA concentration was markedly elevated. In addition, he had a history of orchitis on two occasions, a previously unreported manifestation of HIDS. This report expands the clinical and laboratory features associated with HIDS and serves to emphasize that a normal serum IgD level does not exclude the diagnosis of HIDS.”
Diagnostic value of serum immunoglobulinaemia D level in patients with a clinical suspicion of hyper IgD syndrome – This study found that patients with confirmed mutations on the MVK gene had normal IgD test results. The authors concluded, “The clinical relevance of the IgD measurement for the diagnosis of MKD in our population appears as poor…”
FMF (Familial Mediterranean Fever)
Extensive Thrombosis in a Patient with Familial Mediterranean Fever, Despite Hyperimmunoglobulin D State in Serum – First Adult Case in Korea – This is a case report of a patient with FMF who had elevated IgD.
Familial Mediterranean Fever: association of elevated IgD plasma levels with specific MEFV mutations – This study evaluated 21 FMF patients that had elevated IgD. It was determined that, “homozygotic status for M694V, and to a lesser extent V726A, is associated with increased risk for higher IgD plasma levels, regardless of colchicine use.”
Familial Mediterranean Fever (FMF): from diagnosis to treatment – 13% of FMF patients have elevated IgD and 23% have elevated IgA.
TRAPS (Tumor Necrosis Factor (TNF) Receptor-associated Periodic Syndrome)
The enlarging clinical, genetic, and population spectrum of tumor necrosis factor receptor-associated periodic syndrome – This study mentions that elevated IgD in a TRAPS patient led to a misdiagnosis of HIDS. “The finding of high IgD levels in one of the families with the T50M mutation contributed to an erroneous diagnosis of HIDS. The same error can probably be found retrospectively in the original description of HIDS by Van der Meer et al. In fact, in the current series, a patient who had recurrent inflammatory attacks but no enlarged lymph nodes had a family history (both parents) of autosomal-dominant disease complicated by amyloidosis, all of which suggests a diagnosis of TRAPS rather than HIDS. High IgD levels have been reported in other inflammatory conditions, including FMF; elevated levels were reported in 13% of a group of 80 FMF patients. This highlights the fact that even in the context of hereditary recurrent inflammatory syndromes, an increase in the serum IgD level is not specific for HIDS.”
Falling into TRAPS – receptor misfolding in the TNF receptor 1-associated periodic fever syndrome – “Laboratory findings in TRAPS are in accordance with a typical inflammatory episode: high levels of C-reactive protein, neutrophilia, moderate complement activation, raised mean erythrocyte sedimentation rate, and, in some cases, marginally raised IgA and IgD levels.”
A nephrotic patient with tumour necrosis factor receptor-associated periodic syndrome, IgA nephropathy and CNS involvement – Another TRAPS patient with elevated IgD. “Furthermore, between the fever attacks, the man had elevated IgD (511 IU/ml; normal value: <100 IU/ml), IgA (8.5 g/l; normal value: <4 g/l) and IgG values (18.1 g/l; normal value: <16 g/l). This prompted us to search for genetic variations in the TNFRSF1A and MVK genes. The genetic analyses disclosed a heterozygous T→C nucleotide substitution (c.250T>C) within exon 3 of the TNFRSF1A gene, resulting in the substitution of cysteine (TGT) at amino acid position 55 by arginine (CGT; C55R). In contrast, no pathogenic mutation was detected in the coding exons and in the neighbouring intronic sequences of the MVK gene.”
Tumor Necrosis Factor Receptor–Associated Periodic Syndrome A Novel Syndrome With Cutaneous Manifestations –“Before the identification of MVK as the gene that causes HIDS, the diagnostic criteria of HIDS required IgD levels exceeding 140 mg/L (14 mg/dL) on 2 occasions at least a month apart. However, elevated IgD levels are not specific for HIDS. Approximately 10% to 13% of patients with TRAPS and FMF have elevated serum IgD levels. In addition, a number of other conditions have been associated with elevated serum IgD levels, including IgD multiple myeloma, Hodgkin disease, cigarette smoking, pregnancy, immunodeficiency syndromes, and recurrent infections.9,47,48 Furthermore, some individuals with typical findings of HIDS and mutations in MVK do not have elevated serum IgD levels.”
Recently Identified IgD Related Autoinflammatory Diseases
As researchers continue to identify new autoinflammatory diseases, it’s being discovered that IgD can be in involved in more syndromes that are less understood. These studies below report on two separate families with two novel autoinflammatory disorders. Both presented with high levels of IgD, but did not have mutations in the MVK gene.
A Novel Autoinflammatory Disorder Characterized by Ectodermal Dysplasia, Metaphyseal Chondrodysplasia, Growth Failure and Hyper-IgD in a Single Family – The symptoms included fevers, ectodermal dysplasia, short stature, and failure to thrive.
Identification of a novel monogenic autoinflammatory disease due to mutation in a mitochondrial chaperone protein in a single kindred, and cure with allogeneic haematopoietic stem cell transplantation – “Three affected children in a Pakistani family suffered from a severe and unusual autoinflammatory syndrome, presenting in the first year of life with recurrent fevers, erythema nodosum-like rash, severe oromucocutaneous ulceration, systemic inflammation, and massively elevated serum IgD, without mutation in MVK.”
For many with recurrent fevers, there is not a single test that can give a clear answer or diagnosis. IgD testing can be a piece of the puzzle to consider, but diagnosing a periodic fever syndrome requires careful consideration of all symptoms, lab results, genetic results, other diagnostic tests (hearing tests, eye exams, skin biopsies, xrays, MRI, etc) and response to treatment. Thankfully today, genetic testing is readily available, often paid for by insurance, and not an outrageous expense. The cost is comparable to many other tests and procedures patients need to get a good diagnosis. The Comparison Chart of Systemic Autoinflammatory Diseases is also a valuable tool in helping to guide testing and diagnosis for these conditions.
More References and Resources
- NIH.gov: New Insights into the Enigma of Immunoglobulin D
- American Society of Hematology: Hereditary Periodic Fever Syndromes
- Nature: MVK mutations and associated clinical features in Italian patients affected with autoinflammatory disorders and recurrent fever
- JAMA Network: Tumor Necrosis Factor Receptor–Associated Periodic SyndromeA Novel Syndrome With Cutaneous Manifestations



