
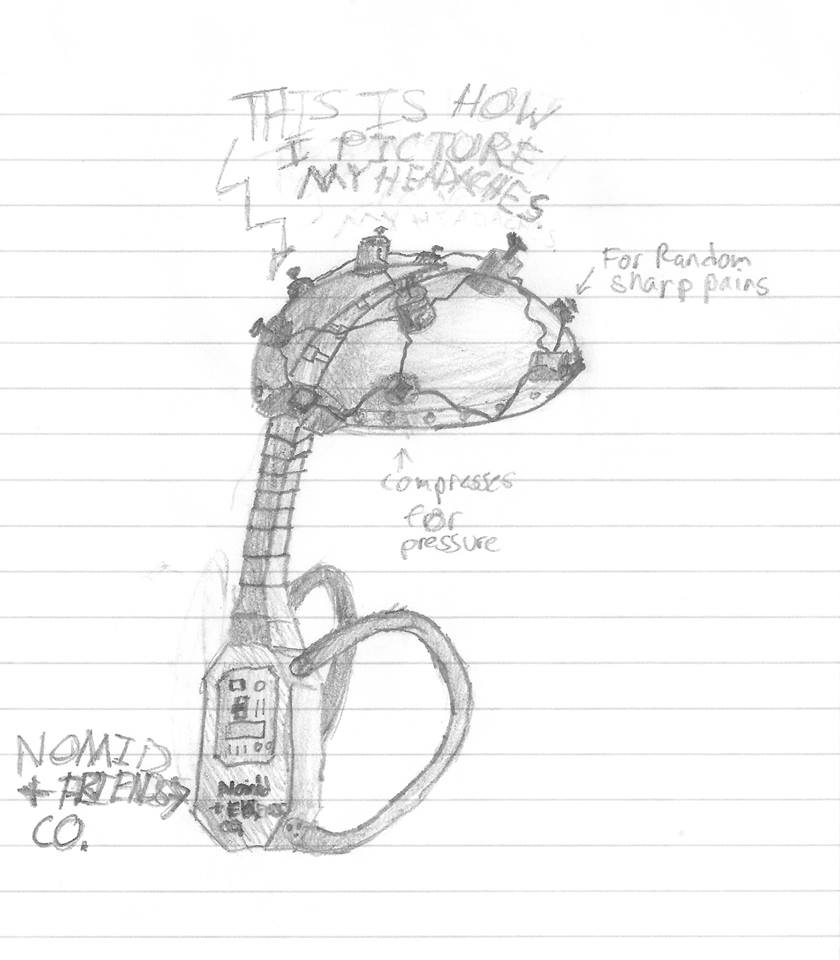
“365 Days of Anakinra Shots.” Virginia was born sick. At just a few days old she had already needed a blood transfusion and surgery, and had unexplained rashes and joint swelling. By 6 months old she got the diagnosis of NOMID and was able to start treatment. Normal for her includes a daily shot, which lets her live a healthier life. Photo by Katherine Buster Whitworth.
Having a chronically sick child means your world gets turned upside down and inside out. You no longer get to live the normal life you once had or imagined for your child and your family. Routines change, friends may change, finances change, and you can feel like life is just chaos.
Nothing seems normal anymore as you spend more of your time with doctors and nurses instead of family and friends; your craft table may now be covered with notebooks and photos documenting symptoms instead of piles of designer scrapbook paper, vacation photos, and glitter pens; you may become more concerned with blood test numbers rather than report card grades, and you read the latest medical literature instead of the latest best seller.
For families dealing with a periodic fever syndrome (aka autoinflammatory disease), watching their child battle recurrent fevers, rashes, joint swelling, and pain becomes part of every day. These symptoms are due to a malfunction of the innate immune system and are not contagious to others. But because these symptoms are debilitating and can appear at any time without warning, it’s hard to make and commit to plans which makes a sense of normalcy seem out of reach. (Learn more about periodic fever syndromes here.)

Koen (who has uSAID), spends a lot of time in hospitals and with doctors. But he still has much to celebrate like being able to attend the first day of high school. When chronic illness works it’s way into normal everyday life, you learn that everyday moments like going to school or attending a birthday party are moments to cherish. Photo by Cat Lichtenbelt.
An invitation to a birthday party, a normal childhood activity, becomes an agonizing decision for a parent. Not because there’s a soccer game at the same time which would be a normal conflict, but because their child may suffer later with flares of fever and joint swelling. Or the excitement of the upcoming party may have already triggered a flare before the party even starts. Do you let them go and do normal kid activities and try to explain to others at the party that they are not contagious, or turn down the invitation and protect them?
This loss of normalcy can make parents and kids feel isolated and grieve the life they knew and had before the illness took over their world.
So how do parents and families find normalcy with a chronically sick child? When does life with a periodic fever syndrome become normal?
Here’s how the experts, who are the patients and parents of patients in our autoinflammatory community, answered the questions.
Our normal is not others’ normal. For years of my kids’ childhoods, and entire lives of previous generations, it was normal to be in pain, covered in rash, and exhausted at the end of the day. It was what it was, and they all assumed there was no treatment – because there wasn’t one until relatively recently. In fact, they didn’t even have a proper name for it. My husband grew up feeling like a weakling because he thought everyone else experienced what he did in cool temperatures.
We’ve had to adjust expectations for our kids from, “You can do anything,” to “Do what you can.”
My kids’ current normal is daily injections that prevent most, but not all symptoms. My husband’s normal is nearly daily symptoms even though he doesn’t work anymore. Our overall normal is tired. So tired.
We’ve had to adjust expectations for our kids from, “You can do anything,” to “Do what you can.”
On the exterior, my family looks normal, and that’s the hardest part. You can’t see their pain and fatigue and anxiety. You can’t tell that their short fuse is due to exhaustion and pain…
Her normal is not my normal – is not her sister’s – nor her dad’s. Even amongst them with the same diagnosis, they have individual normals.
You’ll find a groove and accommodations to make your own normal.
– J.E., FCAS family. Learn more about FCAS, a form of CAPS here.
It’s a journey.
-S.S.H., mom of a child with CAPS. Learn more about CAPS here.
It’s very draining when you’re the main caretaker. For me, what has helped is to have a plan in place for when my son flares. I’ve started taking people up on their offers to help. When my son is sick, my daughter hangs out at the neighbor’s for a break. I’ll drop her off at a friend’s house, or I’ll take my neighbor up on that offer to pick some things up at the store for me. My husband works a lot and travels a lot, so if he’s here, I get out when I can (or I go crazy spending days as a human cushion). He’s understanding as he has an autoimmune condition, so I’m often doing double duty.
For me, what has helped is to have a plan in place for when my son flares. Now I’m finally accepting my “new normal,” like everyone has said, and just planning for it.
-M.K., mom of a child with PFAPA. Learn more about PFAPA here.
Many times, my sons are too sick during uncontrolled flares to participate in much. However, if they insist on not missing out, especially now that they thankfully respond fairly well to treatment, then I listen to them. Their quality of life was so poor when I cared about what others thought (I’m over that now lol) and when I followed normal rules of staying home when unwell. I think I pushed past that notion because hanging out by yourself when chronically unwell stinks. Now we let our boys decide what is best for them, and if they choose to go we explain to family and friends that they are not sick with something contagious.
Their quality of life was so poor when I cared about what others thought (I’m over that now lol) and when I followed normal rules of staying home when unwell. Now we let our boys decide what is best for them, and if they choose to go we explain to family and friends that they are not sick with something contagious.
-K.F.B., mom to twins with uSAID/IFIH1 mutation. Learn more about uSAID here.
We learned a long time ago to let my daughter decide if she feels well enough to participate in activities. Honestly, if we held her back from everything, she would have no enjoyment in life.
-S.T.L, mom of a child with HIDS. Learn more about HIDS here.
We had absolutely NO help for eight years of the hardest times, and even had to downsize to a car from our van, and live in a two-bedroom apartment (with three kids) and it was really bad mentally for me. No treatment, no help, 3 kids flaring all on top of each other. I honestly spent a few years in what I call, “robot mode.” I just did what I had to do to get through it, but didn’t feel like I was living.
My husband is the sole breadwinner, and a firefighter, and also was not aware he had CAPS. So, during that time, he would come home and be exhausted, and had these rashes he was hiding, and having a harder time hearing. All his sick leave was used for the kids. My parents would come to visit, but every single time the kids would end up flaring or getting sick as soon as they left, so it would stress me out more as they would come and ‘have fun’ and then we would be left to pick up the pieces. I think being cooped up in a small apartment is what made it all worse!
I don’t let it get in the way of our fun, but it’s still there, as I know at any moment the kids could get really sick or we could have an issue with the medicine. I know not to take for granted their current health status.
Oddly enough, in some ways I feel luckier to have three kids with CAPS as they all understand each other. If one is feeling bad, the others bring them lunch, set up the tray table, and get the iPad going. Plus, they all have to get the shots, so it was easier to accept that as their normal.
-J.V., family with CAPS. Learn more about CAPS here.
You will find a new normal and as things change with the illness for better or worse you will find another new normal. You lean heavily at times on those who understand and help you through. It isn’t easy but you will discover that you are stronger than you ever imagined, not by choice but by need. You are an amazing person and you will figure it out.
-K.C.
I think sometimes it’s hard to see outside of your own distinct stage in this journey. I remember the beginning of our journey, and I did grieve the loss of healthy children. Sometimes I still slide back there even with a good support system around me. I have learned to take people up on their offers to help. It was hard for me to learn that it’s OK to be the needy one sometimes. That is not my personality…I struggle when I’m not the one giving. However, I have found that while I have the most wonderful tribe of close friends (that group changed some as I did lose certain friends over having sick kids all the time) and a supportive family, that’s been a process. There were times when some family/friends were frustrated hearing about it, like it should be going away by now or something. I learned that my circle of support system was going to be different (and smaller) than I thought, but that the few people in it were going to be absolute rocks to me. They are the ones who can laugh about the ridiculousness of certain doctor appointments with me and who are fine with my kids running fevers at their houses, who treat my kids as kids and who see them for who they are as people, regardless of a possible pretty scary diagnosis. You will figure out who these people are in your life too, but it wasn’t quick for me.
I learned that my circle of support system was going to be different (and smaller) than I thought, but that the few people in it were going to be absolute rocks to me. You will figure out who these people are in your life too.
This rare, chronic world is unfamiliar territory, but it becomes a lot easier to navigate with time.
-K.F.B., mom to twins with uSAID/IFIH1 mutation. Learn more about uSAID here.





 A flare feels like a really bad flu bug – rash, fever, swollen glands, sores in my mouth and throat with a pain throughout my bones. However, because it doesn’t have a name and because I can’t find a doctor who understands how to diagnose this, I am expected to continue preform my life as if I am a healthy person. Worse, as a business woman, I have to keep my illness hidden from my male colleagues so that I do not appear weak and inferior. -C.E., age 42 diagnosed with
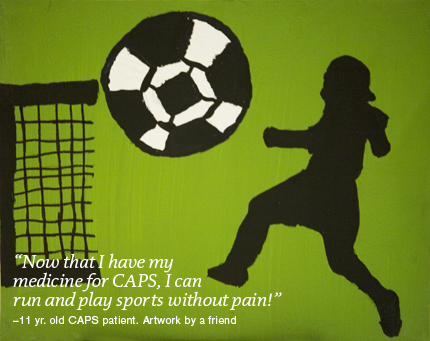
A flare feels like a really bad flu bug – rash, fever, swollen glands, sores in my mouth and throat with a pain throughout my bones. However, because it doesn’t have a name and because I can’t find a doctor who understands how to diagnose this, I am expected to continue preform my life as if I am a healthy person. Worse, as a business woman, I have to keep my illness hidden from my male colleagues so that I do not appear weak and inferior. -C.E., age 42 diagnosed with 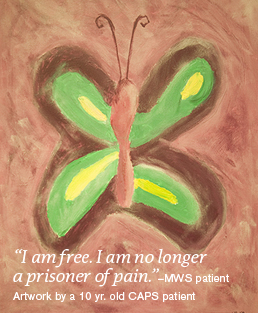 I never knew what “normal” was supposed to feel like until I went on treatment for CAPS. I am free-I am no longer a prisoner of pain. -A.C., diagnosed in adulthood with
I never knew what “normal” was supposed to feel like until I went on treatment for CAPS. I am free-I am no longer a prisoner of pain. -A.C., diagnosed in adulthood with