As news has grown about the hyperinflammation syndrome happening in some children possibly connected with COVID-19, we know many parents of kids with periodic fever syndromes are concerned.
Originally reports came out that this syndrome was similar to Kawasaki Disease, but as doctors and researchers have learned more, this new syndrome has some different symptoms and blood test results than Kawasaki’s. The CDC health advisory here refers to this hyperinflammation syndrome as Multisystem Inflammatory Syndrome in Children (MIS-C), previously named by some researchers as Pediatric Inflammatory Multisystem Syndrome (PIMS).
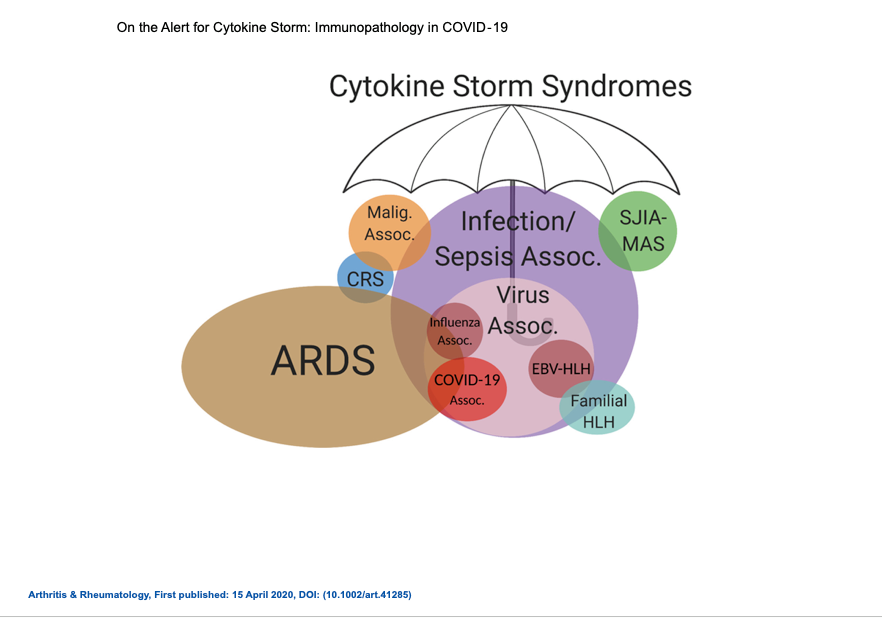
We’ve collected some good and updated information below on MIS-C/PIMS to help learn more about it, as many with an autoinflammatory disease have noticed that it looks like a very bad autoinflammatory disease flare. Hyperinflammation in both adults and children related to COVID-19 infections is thought to be a an overactive immune response to the virus. The hyperinflammation, either during an active COVID-19 infection, or in the case of MIS-C/PIMS, weeks after the COVID-19 infection may cause symptoms similar to the cytokine storms some adults get with COVID, but at this time, it has not been connected to any systemic autoinflammatory diseases (SAIDs).
In fact, a number of reports state that the majority of children that develop MIS-C/PIMS were previous healthy with no pre-existing conditions or chronic illnesses. We are aware that many patients and caregivers are very concerned about the risk for MIS-C in patients with autoinflammatory, or other rheumatic diseases, but at this time, no connection or increased risk has been identified.
Timing of the development of MIS-C/PIMS seems to happen after a COVID-19 infection when antibodies to the virus are developing. According to Dr. Levin of Imperial College in London, “There is a concern that we are seeing a dysregulated immune response…The timing of this illness does seem to coincide with when acquired immunity would be developing.”
MIS-C/PIMS is currently considered very rare, but for those living with a rare autoinflammatory disease, saying something is “rare” may not give much comfort. Knowledge is power, so it is helpful to learn about MIS-C/PIMS, and the symptoms of COVID-19 infections to try and recognize a autoinflammatory disease flare, vs something different. It may be difficult to determine what is a viral-triggered flare, or hyperinflammation associated with COVID-19, or MIS-C/PIMS, so if there are any concerns, it is essential to contact your doctor right away, or seek urgent care or emergency care if you cannot reach your doctors easily.
Here are some helpful guidelines to always remember–no matter what virus is going around, but especially with COVID-19, as we still know so little about it:
If your or your child’s periodic fever/autoinflammatory syndrome symptoms are:
- New = CALL/SEE A DOCTOR (or NP or PA)
- Different = CALL/SEE A DOCTOR (or NP or PA)
- More severe than typical = CALL/SEE A DOCTOR (or NP or PA)
- Not responding to treatment(s) as would be typical = CALL/SEE A DOCTOR (or NP or PA)
- Concerning to you = CALL/SEE A DOCTOR (or NP or PA)
In one of the articles posted below, one doctor stated, “Because parents are afraid of coming to the hospital, they may delay bringing sick children in, which can lead to serious complications…” So, don’t be afraid to go to the ER when needed.
With COVID-19, and MIS-C/PIMS, patients can quickly become more sick, so consider calling for EMS (911 in the US) for an ambulance, if you or your child/loved one is having increased difficulty breathing, responding, or you are not confident you can drive yourself, or your loved one safely to the hospital for urgent care.
Do Children with Autoinflammatory Diseases Have an Increased Risk for MIS-C/PIMS?
We don’t know at this time. The answer is the same as for adults with autoinflammatory diseases, and the risk of a COVID cytokine storm; There’s no research to help answer this question at this time. The virus is just too new, and with autoinflammatory disease being rare, there’s very little known. If you have concerns, contact your doctor regarding your concerns and risks.
The Expert/Autoinflammatory/Rheumatology organization statements here have more guidance on managing your autoinflammatory disease and possible risks in regards to COVID-19. We are adding and updating the list regularly, as the care and treatment for COVID-19 is emerging.
Also, if you or your child with an autoinflammatory disease does get diagnosed with COVID-19, please encourage your doctor to register them with Rheum-COVID.org. This is how we can all best learn about autoinflammatory diseases and COVID-19. You can also complete the Patient Experience Survey on the rheum-covid.org page at this link, to report yours or your child/loved one’s experience with COVID (diagnosed with testing, or clinically based on symptoms.)
“PIMS stands for pediatric inflammatory multisystem syndrome [now referred to as MIS-C]. It describes a new health condition seen in children who have been infected with novel coronavirus, recovered from it and later have an immune response that results in significant levels of inflammation in organ systems and symptoms. PIMS is similar to other inflammatory conditions like Kawasaki disease and toxic shock syndrome.
Children who have PIMS generally did not have obvious symptoms when they were infected with novel coronavirus, like cough, and generally were healthy prior to developing PIMS.”
Kids with suspected COVID-related syndrome need immediate attention, doctors say
“The syndrome appears to develop two to six weeks after infection with Covid-19 and affects mostly children who were perfectly healthy beforehand.”
“”Any child at home who has fever, abdominal pain or symptoms such as rash and conjunctivitis should be seen by a pediatrician right away,” he advised. “I think we need to have a low threshold for evaluation.”
“And most of the children had no underlying conditions that might make parents wary. “No definitive underlying conditions predispose children to this,” he said.”
Mystery Inflammatory Syndrome in Kids And Teens Likely Linked To COVID-19
“The inflammatory syndrome can appear days to weeks after COVID-19 illness, doctors say, suggesting the syndrome arises out of the immune system’s response to the virus.
“One theory is that as one begins to make antibodies to SARS-COV-2, the antibody itself may be provoking an immune response,” says Newburger.”
“”They all present in varying ways,” says Parikh, who is also a spokesperson for Physicians for Patient Protection. “But the common theme was fever and rash. One had very, very swollen lymph nodes and lymph glands. And then, aside from that, they had markers of inflammation elevated in their blood.””
15 states now investigating child illness possibly linked to coronavirus, Cuomo says
“COVID-19 symptoms are predominantly respiratory; but the Kawasaki-like syndrome [now referred to as MIS-C] seen in children appears to be caused by an inflammation of blood vessels, presenting cardiac symptoms. Predominant symptoms include prolonged fever, abdominal pain and a skin rash. Afflicted children, however, have also shown had changes in skin color (becoming, pale, patchy, or blue), difficulty feeding (for infants), difficulty breathing, a racing heart, as well as lethargy, irritability or confusion. “
Severe COVID-19 in Children and Young Adults in the Washington, DC Metropolitan Region – Published in The Journal of Pediatrics
This is a detailed overview of 177 children and young adults with PIMS. It includes details of symptoms, ages, underlying medical conditions and more.
The authors noted in the results:
With regard to symptoms, shortness of breath was more common in hospitalized compared with non-hospitalized children/young adults, but other features did not clearly distinguish them from less ill children, including presence of fever. Minor symptoms such as congestion/rhinorrhea, sore throat, cough and headache were also present more commonly in the non-hospitalized cohort. As has been the case in adult reports, fewer than half of the patients had both fever and respiratory symptoms present at the time of their diagnosis, but the majorities have one or the other. Our critically ill cohort includes a previously well child with the newly emerged hyper-inflammatory phenotype of SARS-CoV-2- associated KD-like shock syndrome [now referred to as MIS-C] that has been identified concurrently within the same time frame at other centers internationally.
Rethinking COVID-19 in Children
“Dr. Newburger said that the Covid-19-related cases are a multisystem severe inflammatory syndrome modulated by the immune system, which many people think may appear a few weeks after the initial encounter with the coronavirus. The children come in with high fevers, with dysfunction in one or more body organs, and with lab tests suggesting inflammation.”
“Because parents are afraid of coming to the hospital, they may delay bringing sick children in, which can lead to serious complications, he said.”
Kawasaki’s Disease and PIMS/MIS-C
Since some children with an autoinflammatory disease have a history of a Kawasaki Disease (KD) or an incomplete KD diagnosis, it’s reassuring that various KD organizations, such as Societi Foundation The UK Kawasaki Disease Foundation and Kawasaki Disease Foundation, have stated the following:
“There is no information to suggest that children who have had KD are at increased risk for complications of COVID-19 infection compared to the general population. Our team at Rady Children’s Hospital San Diego and UCSD are at the forefront of research to understand this new, complicated form of COVID-19/KD and are collaborating with colleagues around the country and around the world to better understand this condition and how to treat it.” – Dr. Jane Burns
“There is no current evidence of any increased incidence or greater susceptibility to Covid-19 infection for children who had Kawasaki Disease in the past.” – Societi Foundation