Below are links to Familial Mediterranean Fever (FMF) studies regarding symptomatic patients who only have one mutation found for FMF. These are not all the studies available however. For more search Pubmed.gov. You can also find links to more FMF research and information here.
Booty et al, “Familial Mediterranean Fever with a Single MEFV Mutation: Where Is the Second Hit,” Arthritis & Rheumatism, 2009: Their “data underscore the existence of a significant subset of FMF patients who are carriers of only 1 MEFV mutation and demonstrate that complete MEFV sequencing is not likely to yield a second mutation. Screening for the set of the most common mutations and detection of a single mutation appears to be sufficient in the presence of clinical symptoms for the diagnosis of FMF and the initiation of a trial of colchicine.”
Kastner et al, “Autoinlfammatory Disease: A Clinical Perspective,” Cell, 2010: “The second “frequently asked question” concerns FMF in particular and is based on the fact that many of the patients with colchicine-responsive clinical FMF have only a single demonstrable MEFV mutation, despite thorough scrutiny ( Booty et al., 2009, Marek-Yagel et al., 2009 and Ozen, 2009). Although this widely confirmed observation is based on a clinical definition of FMF that includes milder cases than were appreciated 20 years ago, it suggests a more complex pattern of inheritance than the simple recessive model of the textbooks. It also argues that solitary MEFV mutations may confer a biochemical or clinical phenotype by mechanisms yet to be elucidated, perhaps in the presence of as yet unidentified modifier loci.”
Ozner Changing concepts in familial mediterranean fever: Is it possible to have an autosomal-recessive disease with only one mutation? Arthritis & Rheumatism, 2009: “Since the identification of the MEFV gene, the mutations have been studied extensively in affected people. Surprisingly, it has become evident that the mutation in the second allele cannot be demonstrated in ∼20–26% of the patients who have FMF (5–7). The phenotype of these patients is confirmed by the presence of typical attacks of FMF symptoms and by the response to colchicine therapy. So, how can a person carrying only 1 MEFV mutation present with this autosomal-recessive disease? Two articles published elsewhere in this issue of Arthritis & Rheumatism address some of the questions in this context.”
Marek-Yagel et al Arthritis & Rheumatism 2009: “These findings are highly consistent with the existence of a clinical phenotype among some patients who are heterozygous for FMF and could explain the vertical transmission in some families. A single mutation in the MEFV gene may be much more common than was previously thought and may include up to 25% of patients who are diagnosed as having FMF.”
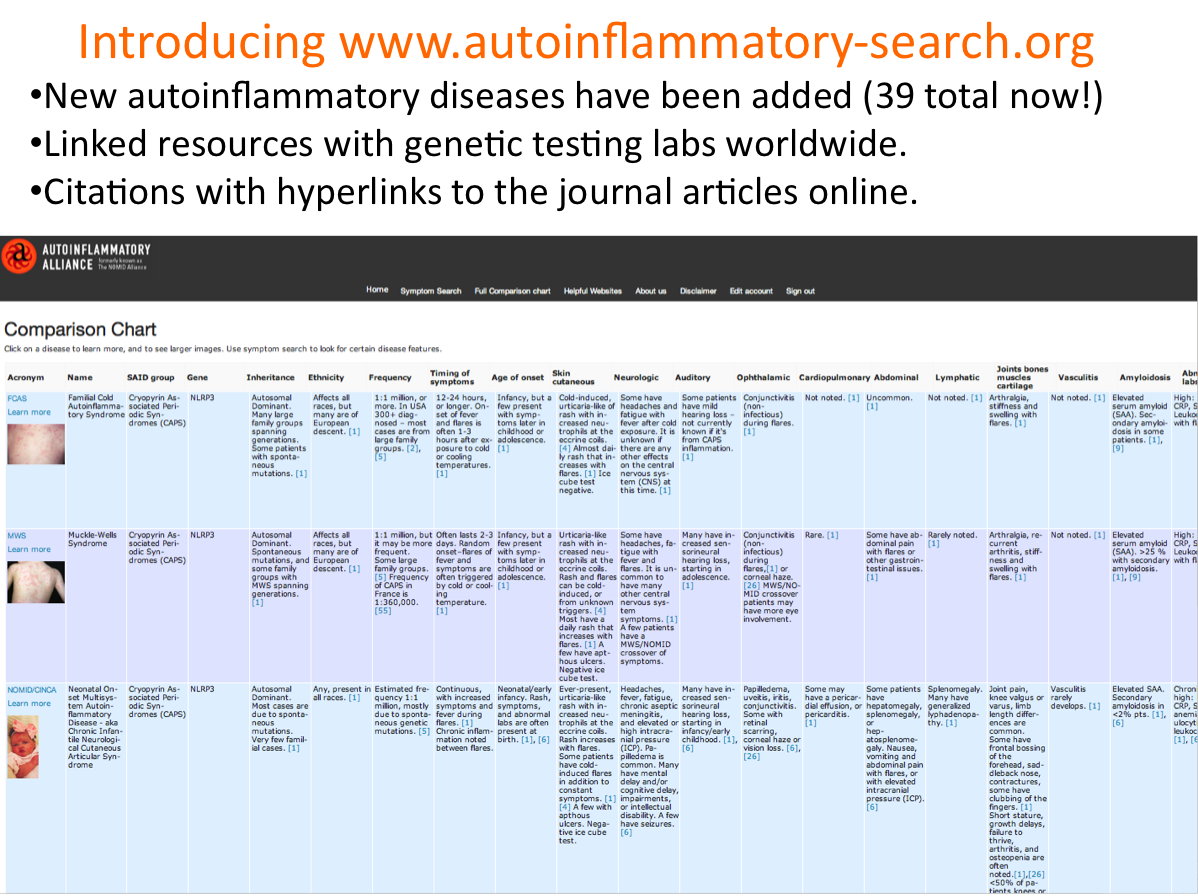
Touitou J Medical Genetics 2013: “Over 15 years have passed since the discovery of the first autoinflammatory gene, MEFV, responsible for familial Mediterranean fever. The identification of another gene, TNFRSF1A, in 1999 led to the concept of autoinflammation which characterises rheumatological conditions triggered by a defective innate immunity. Substantive progress has been made since then with the identification of 18 autoinflammatory genes accounting for up to 24 disease entities showing overlapping symptoms. The accumulation of studies reporting patients with missing or excess mutations as compared with expected numbers favours the hypothesis that these diseases are distributed along a continuum ranging from monogenic to multifactorial conditions, rather than featuring only classical modes of inheritance. Moreover, the probable interactions of environmental and epigenetic factors further obscure our understanding of the mechanisms underlying the phenotypic expression of patients. This review explores the history of autoinflammatory gene discovery, discusses the nosological disparities stemming from the clinical versus pathophysiological definition of autoinflammatory diseases and summarises various inheritance patterns. This review calls for a consistent disease nomenclature and presents a reconciling hypothesis which places different sequence variants within the autoinflammatory disease continuum. Integrating these new concepts should help to facilitate communication between health professionals and promote personalised patient care.”
Kone-Paut et al (Rheumatology, 2009): Assessed clinical characteristics of 94 French patients carrying single MEFV mutation. “The clinical picture of French heterozygote patients with recurrent fevers resembles that of homozygote patients.” Most of them required colchicine treatment. Fever > 39 C (80%), duration (1-3 56%, > 3 days 36%), frequency (1-2 months 48%, > 2 months 15%), peritonitis (97%), pleuritis (25%), athralgia (53%), skin rashes (20%), apthosis (18%), lymphadenopathy (9%). MEFV mutations were MEF94 (60%), M694I (7%).
Federici (Annals of Rheumatology Disease, 2012): Comparisons of children with two MEFV mutations, one MEFV mutation, and no mutations. “This clinical observation supports recent findings contrasting the notion of FMF being a pure autosomal recessive disorder associated with recurrence of mutations leading to loss of protein function. A dosage effect could be invoked, giving rise to symptom onset even in the presence of one wild-type allele.”
Moradian et al (Journal of Human Genetics, 2010): Study of 1299 Armenian patients including 236 (18%) with definitive diagnosis of FMF. From these selected individuals with two mutations and single mutation along with non-clinical control group. Compared symptoms of double mutation individuals with other two groups. “We found extremely high probabilities for the presence of FMF symptom in heterozygous [single mutation] idnviduals and determined that symptoms were eually likely to occur in both analyzed genotypes (double and single mutation). Therefore, our study supports the rising evidence that a single MEFV mutation could be associated with mild FMF symptoms.”
Bardeli et al (Genetic Testing and Molecular Biomarkers, 2011): Using DNA sequencing …”Familial Mediterranean fever (FMF) is a hereditary autoinflammatory disorder characterized by episodes of inflammation in the absence of high-titer autoantibodies or antigen-specific T cells. The Mediterranean fever (MEFV) gene located on chromosome 16p13.3, which encodes the 781–amino-acid protein pyrin, is the causative gene for this monogenic Mendelian disease. This study presents the molecular analysis of an MEFV gene mutation screen of 5518 Turkish individuals with clinical diagnoses of FMF. Patients were genetically diagnosed using the FMF StripAssay and DNA sequencing analysis. Contrary to the results achieved by the FMF StripAssay, DNA sequencing analysis identified large-scale coding and noncoding novel sequence variants, together with a significant group (76%) of individuals who were receiving colchicine and had a single heterozygous mutation, despite the recessive inheritance of FMF. In conclusion, sequence analysis, unlike other routine laboratory techniques, may enable screening for a broad range of nucleotide variations and may prevent less common, population-restricted, novel sequence variants from being overlooked.”