 Updated 4/13/2022
Updated 4/13/2022
Familial Mediterranean fever (FMF), PFAPA syndrome, cryopyrin-associated periodic syndromes (CAPS), hyperimmunoglobulinemia D with periodic fever (HIDS), or other autoinflammatory diseases probably did not make the news last night. These diseases are rare and largely unheard of except by those suffering from them and their close family and friends. Because of their rarity and lack of attention, many family, friends, and even medical professionals, do not have a full understanding of these conditions, and often believe many myths and misconceptions about them.
Here are some of the common myths or misconceptions about periodic fever syndromes that patients often encounter and information to help better understand these conditions.
Myth 1: “If the fever responds to a single high dose of prednisone, it must be PFAPA.”
FALSE
Other fever syndromes besides PFAPA will respond to prednisone, often with just a single dose. HIDS (hyper-IgD syndrome) is one autoinflammatory disease that may respond to a single dose of prednisone in some patients and the two diseases have very similar symptoms and fever patterns.
In fact, the recommended use of prednisone and response to prednisone can be exactly the same for HIDS and PFAPA. In both, the recommended starting dose is 1 mg/kg at the onset of the flare. In many patients with HIDS and with PFAPA, the fever and other symptoms will fade away within a couple of hours after taking prednisone. Some with both HIDS and PFAPA will need another dose the next day. In some with HIDS and some with PFAPA, prednisone will bring the flares closer together. Click here for prednisone use in PFAPA and for HIDS.
Response to prednisone by itself is not diagnostic to PFAPA, but can be helpful in narrowing down which autoinflammatory disease to consider for diagnosis. If the fever and symptoms respond to a single dose of prednisone, then both PFAPA and HIDS should be considered for diagnosis, but know that other autoinflammatory conditions, such as TRAPS, may also respond to prednisone treatment. Some with undifferentiated autoinflamamtory diseases may also respond well to prednisone. Click here to compare symptoms of PFAPA, HIDS, FMF, TRAPS, and other similar fever syndromes.
Myth 2: “It’s just a fever. Maybe it’s just a virus”
FALSE
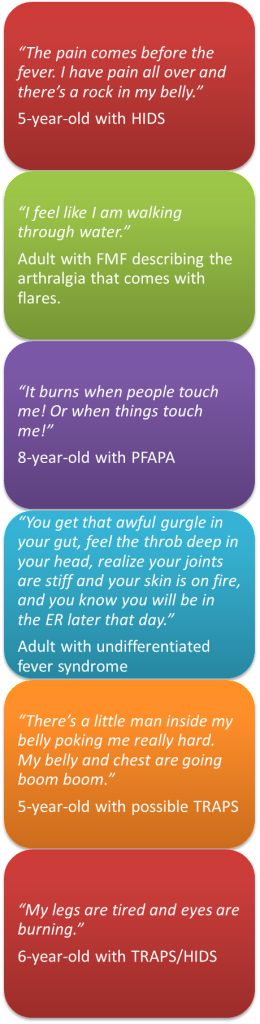
Many well-meaning family, friends, and even medical professionals may say, “maybe it’s just a virus” and “kids do get fevers.” Even if a virus triggered the flare, a flare is nothing like your average virus or childhood fever most kids experience.
High fevers can evoke great fear and concern, so it is important to rule out infections as the cause when seeking a diagnosis for unexplained fevers. Many patients with periodic fever syndromes initially experience a number of visits to the doctor and lots of tests, before they notice a pattern of symptoms with the fever in the absence of infection with each episode.
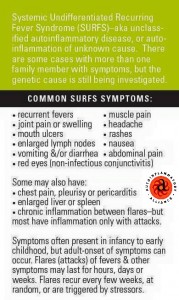
Although the fever, which in some conditions can reach over 105 degrees F, is the most prominent and easily measured symptom in many periodic fever syndromes (and gave rise to the name periodic fever syndromes), it is often the least concerning symptom in regards to overall inflammation. Periodic fever syndromes are systemic inflammatory diseases that affect the entire body, and the fever is just one sign that the body is in a state of overall inflammation. The inflammation occurs throughout the body and can affect any organ system. Different autoinflammatory diseases may have certain organs and tissues that present with more obvious signs of inflammation, so keeping track of symptoms is essential.
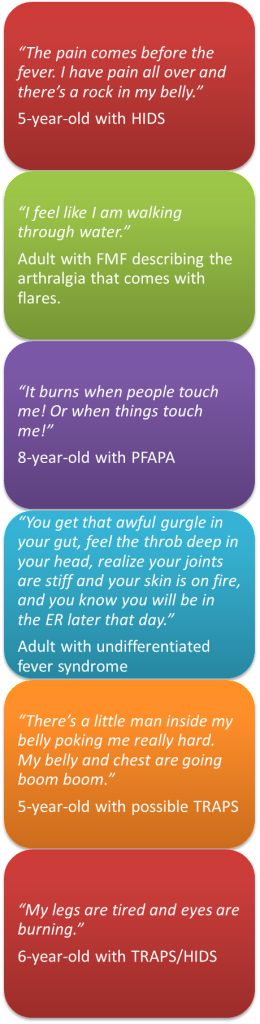
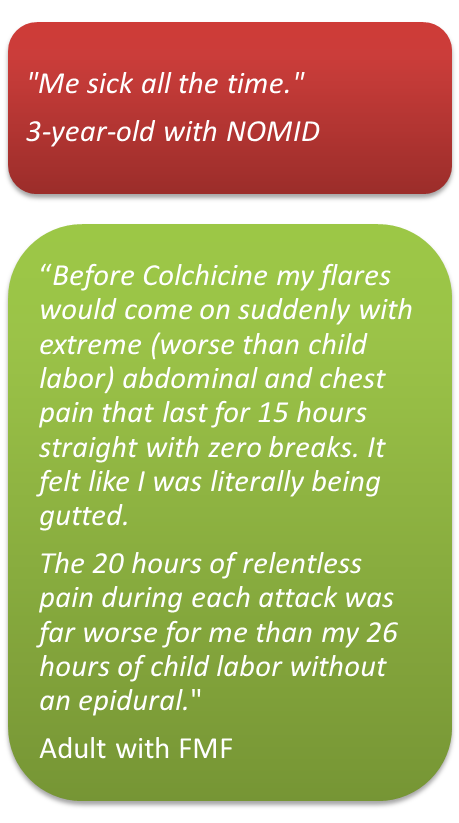
When the fever hits, flares of autoinflammatory disease symptoms that can accompany the fever can include: joint swelling, rashes, bone pain, inflammation in the eye, vomiting, inflammation in the abdominal cavity, inflammation around the heart, headache, muscle pain, plus many other symptoms that may also affect the patient simultaneously. For some conditions, this inflammation is chronic without periods of relief of symptoms. In some, the severity of symptoms may vary in intensity and pain from mild/moderate to severe, even within a weekly or monthly period of time. Chronic inflammation from systemic autoinflammatory diseases can cause patients to feel like their body is “out of control” or in “chaos.” Long-term systemic inflammation from some of these diseases can cause more serious health issues, such as kidney damage, hearing loss, and vision problems, and some can be fatal. These diseases are not just a fever.
For all patients, the unpredictability and frequency of the symptoms and flares can cause great psychological stress and challenges and for the family. Since these are lifelong diseases in most cases, this can be a great concern for quality of life, socialization, school, and work.
Patients with a periodic fever syndrome (systemic autoinflammatory disease) will still have time when they have a fever due to a true infection and can have infections and flares at the same time. And this can complicate things even more. Keeping a symptom diary helps you recognize when symptoms “fit” the usual flare symptoms, or if there may be another cause for the symptoms. Take the patient to the doctor or the ER immediately for any change in consciousness, seizure, difficulty breathing, blue lips, if they are unable to keep fluids down, are not producing urine for most of the day, or if you feel that something is wrong. Listen to your “gut instinct” and know that there is never anything wrong with having a doctor check your child, or yourself in these situations.
Here is a helpful list of fever facts vs. myths from St. Louis Children’s Hospital that will help to dispel a number of concerns and misconceptions about fevers from normal illnesses.
Myth 3: “If you don’t have every symptom of X, Y, or Z fever syndrome, then you don’t have that autoinflammatory disease.”
FALSE
Patients with any of the known autoinflammatory syndromes will have a majority of the symptoms of that disease, but not always all of them. A number of these diseases have a range of severity, and a few also have variant forms of the disease, so it is essential to look at the list of symptoms and lab results collectively.
When making a diagnosis, several things need to be considered together to make the best diagnosis. Lab tests, biopsies, evaluation of symptoms, eye and hearing tests, plus other diagnostic tests like an x-rays, or an MRI, may help aid the diagnosis, along with genetic testing for suspected autoinflammatory diseases. In some cases, individual patients may never develop certain symptoms, or they may develop these problems later in life. In some of the more severe and chronic autoinflammatory diseases a few symptoms, such as amyloidosis, may only develop in patients that have not been on medications to treat their disease for most of their life. And some patients will have other symptoms that may not be on the list for a certain disease, due to variant presentations of their disease that have not been documented, or because they may have a concurrent disease affecting them, so it is important to look at the whole picture. Not having vomiting or diarrhea does not mean it can’t possibly be HIDS. Not having a rash does not mean it can’t possibly be any autoinflammatory syndrome.
We have heard from a number of patients with CAPS who had the rash, fevers/chills (but not necessarily high fevers), red eyes and hearing loss, but the doctors never connected these symptoms as all being possibly from the same disease for many years! All are classic symptoms of Muckle-Wells syndrome (MWS)–a form of CAPS. The doctors were treating each symptom separately, and not looking to see if these could all be connected. Once the patients are diagnosed with their disease, a lot of things start to fall into place that were initially considered unrelated.
Myth 4: “They will outgrow it.”
In most cases, this is FALSE. For some, the answer could be MAYBE, and for very few autoinflammatory diseases, this could be TRUE
Most autoinflammatory diseases will not be outgrown as they are lifelong diseases, so their answer would be FALSE to this myth. Many are caused by known genetic mutations in the person’s DNA that will not change, so patients will live with these symptoms their entire life. In some cases, symptoms may lessen as patients get older, but in other diseases, symptoms may start to appear, or become worse as the patient ages.
There are some cases of periods of remission of symptoms for some autoinflammatory diseases, such as with FMF, TRAPS, Behçets and a few others, but most patients have symptoms of their disease throughout their life. So, for some conditions, MAYBE would be a possibility, but it may give false hope to tell patients this, as it is not the norm for most of these diseases, and while some disease may have periods of remission symptoms can return, especially during stressful periods in life.
Some patients may have more severe disease as they get older. A number of patients with CAPS and FMF have expressed greater severity, and challenges with their disease as they have grown up. Also with these severe systemic autoinflammatory diseases, lifelong chronic inflammation can cause damage to various organs if left untreated for years. This is true for a number of autoinflammatory diseases.
PFAPA is one exception. This is the only autoinflammatory disease where one could say that most patients will outgrow it. Studies show that most patients with PFAPA will outgrow their condition by the early teen years. One study showed that 90% with a PFAPA diagnosis outgrew PFAPA at an average of 6.3 years after symptoms started. However, this is for cases that truly have PFAPA. There are a number of cases where patients were initially diagnosed with PFAPA, that were finally found to have the correct diagnosis of another autoinflammatory disease (often TRAPS, FMF, CAPS or HIDS), after the patients continued to have their symptoms into their teens, or did not respond to the recommended PFAPA treatment of removing the tonsils.
In HIDS studies, some adults have milder or fewer flares as adults, but this does not happen for every HIDS patient and for most, symptoms do not completely disappear. In some cases, adults may experience additional complications from their disease.
Please understand, especially for those who may eventually outgrow their condition, that if they are currently suffering, they are in great pain and agony during their flares, and deserve good treatment and compassion, because these diseases are “not just a fever.”

Conjunctivitis can be a symptom of TRAPS, CAPS, and other autoinflammatory syndromes, but it is NOT contagious with these conditions. Photo by soupstock/BigSTockPhoto.com
Myth 5: “Symptoms are contagious.”
FALSE
The rash, mouth ulcers, fever, conjunctivitis, and all other symptoms of autoinflammatory diseases are never contagious. They are produced by the individual’s immune system and cannot be spread to anyone else. Often, CAPS patients are prescribed eye medications for their frequent, persistent non-infectious conjunctivitis, and the doctors are baffled that none of the ophthalmic medications that they are prescribing work!
It is essential for schools and other facilities understand that if a patient has one of these autoinflammatory diseases (and does not have any signs of infection from a concurrent disease), that they are NOT at risk of spreading an infection, and should be allowed to remain at school if they have non-infectious conjunctivitis, a fever, or mouth sores. Also, the red, glassy eyes are due to an autoinflammatory disease, and not the use of an illegal drugs either!
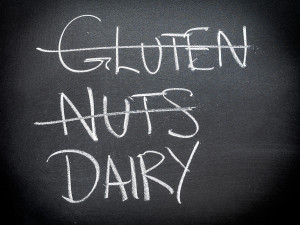
Foods do not cause autoinflammatory diseases. Photo by photosquared/Bigstockphoto.com
Myth 6: “It must be an allergy. Stop eating diary, wheat, gluten, MSG, etc and you will be fine.”
FALSE
Patients with autoinflammatory conditions are not causing their symptoms due to what they eat or their lifestyle. The conditions are caused by a malfunction the immune system that is often due to a genetic mutation.
No diet or food will fix a mutation in the DNA. Some patients, but not all, may also have allergies or intolerances in addition to their autoinflammatory condition, or have gastrointestinal symptoms as part of their condition. In some patients, (but not all) controlling their allergies and GI symptoms may provide some relief from those individual symptoms, but it does not cure them of or treat their autoinflammatory disease. Click here to read more about diet and lifestyle for periodic fever syndromes. Be aware that some medications that may be prescribed to treat an autoinflammatory disease could be the cause of any issues with intolerences, such as colchicine leading to increased lactose intolerence.
In addition, many patients have seen allergy doctors, especially if they have had rashes with their disease. It is very common for patients to get referred to a few different types of doctors when seeking a diagnosis. Many have tried elimination diets, or other measures to reduce presumed allergies, with no success–unless they were found to have a concurrent allergy that needed to be treated in addition to their autoinflammatory disease.
Myth 7: “They need to build their immunity – that’s why they keep getting fevers.”
FALSE
Actually it’s quite the opposite. Patients with autoinflammatory conditions have a very robust immune system, that is in many ways, “too robust.” Their innate immune system is ready at all times to tackle any virus, bacteria, or any suspected offender to the body. The innate immune system in fever syndromes overreacts, and often just reacts without cause or control producing severe inflammation in the entire body. In some of these diseases, such as CAPS, the innate immune system it is activated and producing substances constantly, such as Interleukin-1β, in the absence of any typical infectious triggers, so patients can have chronic inflammation in their bodies. Read this article to better understand what is happening to the immune system in autoinflammatory conditions.
For more on this, also see above for myth #2 “it’s not just a fever, nor is it just a virus.”

DNA photo by Mike_Kiev/Bigstockphoto.com
Myth 8: “If genetic tests are negative, then it must be PFAPA.”
FALSE
Several periodic fever syndromes can have the same symptoms and fever pattern as PFAPA. These include FMF, HIDS, TRAPS, TRAPS11, and CAPS among others. Genetic testing is an important tool to help determine which fever syndrome a patient might have. However, if genetic testing is negative for similar conditions, it does not automatically mean the diagnosis is PFAPA. A PFAPA diagnosis is made by using the PFAPA diagnostic criteria.
A key feature of the PFAPA diagnostic criteria is that flares are very predictable and cyclic without triggers. PFAPA also involves elevated CRP and ESR labs and symptoms being present only during flares, with no signs of chronic inflammation between flare episodes. So, if a patient has elevated inflammatory marker labs (ESR, CRP) when the patient has no fever, or other symptoms, such as joint swelling, it would be incorrect to label a patient as having PFAPA even if genetic testing is negative. It is hard to not want to give a patient a diagnosis, and of all the autoinflammatory diseases, PFAPA may be the most reassuring diagnosis, as patients can outgrow it, and it is not associated with chronic inflammation or organ damage. But the misdiagnosis of PFAPA has led may patients to having delayed access to beneficial treatment for their disease that could have prevented or lessened systemic damage.
One study found up to 20% of patients that met the initial criteria for PFAPA were found to actually have NLRP3 variants, a genetic autoinflammatory disease. Another study showed almost 40% initially diagnosed as PFAPA had a positive genetic test for HIDS, FMF, or TRAPS. These studies show how PFAPA can easily be misdiagnosed.
When genetic testing is negative and a patient does not clinically fit a known autoinflammatory disease, then they can be diagnosed with undifferentiated autoinflammatory disease. Read more here.
Genetic testing only looks for mutations on the genes known to be associated with these conditions. It’s possible that not all genes or mutations have been discovered for any of these conditions. Patients can be diagnosed clinically for HIDS, TRAPS, CAPS, FMF, and others, even if their genetic testing was negative. Some genetic testing panels only test for mutations in certain exons, or for the more common areas for these diseases, so uncommon, or unknown mutations could be missed.
With some forms of CAPS, the older standard genetic testing did not identify mutations in around 40% of cases–often in the most severe form of CAPS, known as NOMID/CINCA. These patients had all the clinical findings, labs and symptoms of NOMID, but were previously called “mutation negative.” In recent years, new methods for testing these patient’s genetics have been developed, and have found somatic mutations for CAPS in around 99% of these patients that were previously considered to not have a known mutation for this disease. Advances in genetics could lead to finding mutations in other patients that were previously considered “mutation negative.” For a detailed discussion on somatic mosaicism in CAPS, and research, please visit this page on our website.
If genetic testing for similar conditions to PFAPA are negative, a diagnosis needs to be made clinically with a careful evaluation of symptoms, response to treatment, and labs. The SAID Database is a helpful tool for this.
Myth 9: “Genetic Testing is Too Expensive and Insurance Won’t Pay for It.”
Mostly FALSE, but sometimes TRUE
There are different types of genetic testing that can be done to help with a periodic fever syndrome diagnosis. Sometimes insurance will pay for these tests without any prior approval. Some plans will need a pre-authorization to cover genetic testing. Sometimes patients and doctors will need to file an appeal to get the testing paid for. As for cost, genetic testing today is inexpensive when compared to many other tests and hospital procedures you or your child have probably had done already. And once a good diagnosis is achieved, which genetic testing can help with, you may save your insurance company money by having better management and treatment of your disease.
In the U.S. there are several labs with fever panels that test for multiple fever syndromes at once. All of these labs are excellent, and these tests, as of 2022, and most larger panels cost less than $1,000. Invitae’s panels are only $250 if using the self pay option. Also, most of the labs offer payment plans, or have other patient assistance plans if you have to pay out of pocket. Click here to learn more about genetic testing for periodic fever syndromes in the U.S.
For some other conditions that are not covered in these periodic fever panels, the doctor can look for specific labs for the suspected disease(s) on the GTR: Genetic Testing Registry. One of the most comprehensive labs for genetic testing for autoinflammatory diseases in Europe is in Genomic Diagnostics Laboratory-University Medical Center Utrecht, Netherlands. Their Autoinflammatory Panel tests for 19 autoinflammatory diseases and their variants! If you live in a country that does not have genetic testing for these diseases, The EUROFEVER Project has a special program.
Some patients require whole genome sequencing, which can cost $5,000 or less. Some other genetic tests are also available through your regular lab or research facilities. Depending on the study protocol and funding, some study participants may have genetic testing done for free.
The only way to determine if your insurance will pay for the genetic testing you need is to call and ask the insurance company. And keep in mind that a denial can always be appealed.
Myth 10: “There are no treatment options.”
FALSE
All of these conditions have treatment options. A few autoinflammatory diseases have FDA-approved medications, such as for FMF and CAPS. But most treatments for autoinflammatory diseases may be ordered “off-label,” meaning that the medication has not been officially developed or approved for that specific disease, but often research has been done with these off-label medications that have found that they may be helpful in treating an autoinflammatory disease. Off-label use of medications is very common in treating many rare diseases. It is best to discuss all the available treatment options with your doctor, and the research behind the options that you are presented. The good news is that there are medications that have been found to treat a number of autoinflammatory diseases. Although patients are not “cured” of their disease, they can often have a healthier life, and improved quality of life with the right treatment. In some conditions, treatments are limited and/or not very successful, but researchers around the world are continuing to look for better treatments. Unfortunately, some medications are not always easily available due to costs, insurance issues, or lack of certain biologic medications in some countries.
The Autoinflammatory Alliance is a 501(c)(3) non-profit organization dedicated to helping those with autoinflammatory diseases.
Donate now to help with awareness, education, and research for these rare diseases.
References
- Orpha.net: Hyperimmunoglobulinemia D with periodic fever
- DermNet NZ: Hyperimmunoglobulinemia D with periodic fever syndrome
- HIDS.net: Treating the disease
- NEJM Journal Watch: Follow-up of Children with PFAPA Syndrome
- Italian Journal of Pediatrics: Autoinflammatory syndromes: diagnosis and management
- All Children’s Hospital Johns Hopkins: Fever – Myths Versus Facts
- Periodic fever, aphthous stomatitis, pharyngitis, cervical adenitis syndrome is linked to dysregulated monocyte IL-1β production.
*Top left photo by stari/Bigstockphoto.com


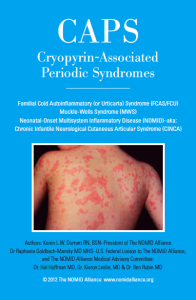 CAPS Guidebook
CAPS Guidebook