This is a collection of research and information on chronic recurrent multifocal osteomyelitis (CRMO). It is not all inclusive. You can search for more studies at PubMed.gov.
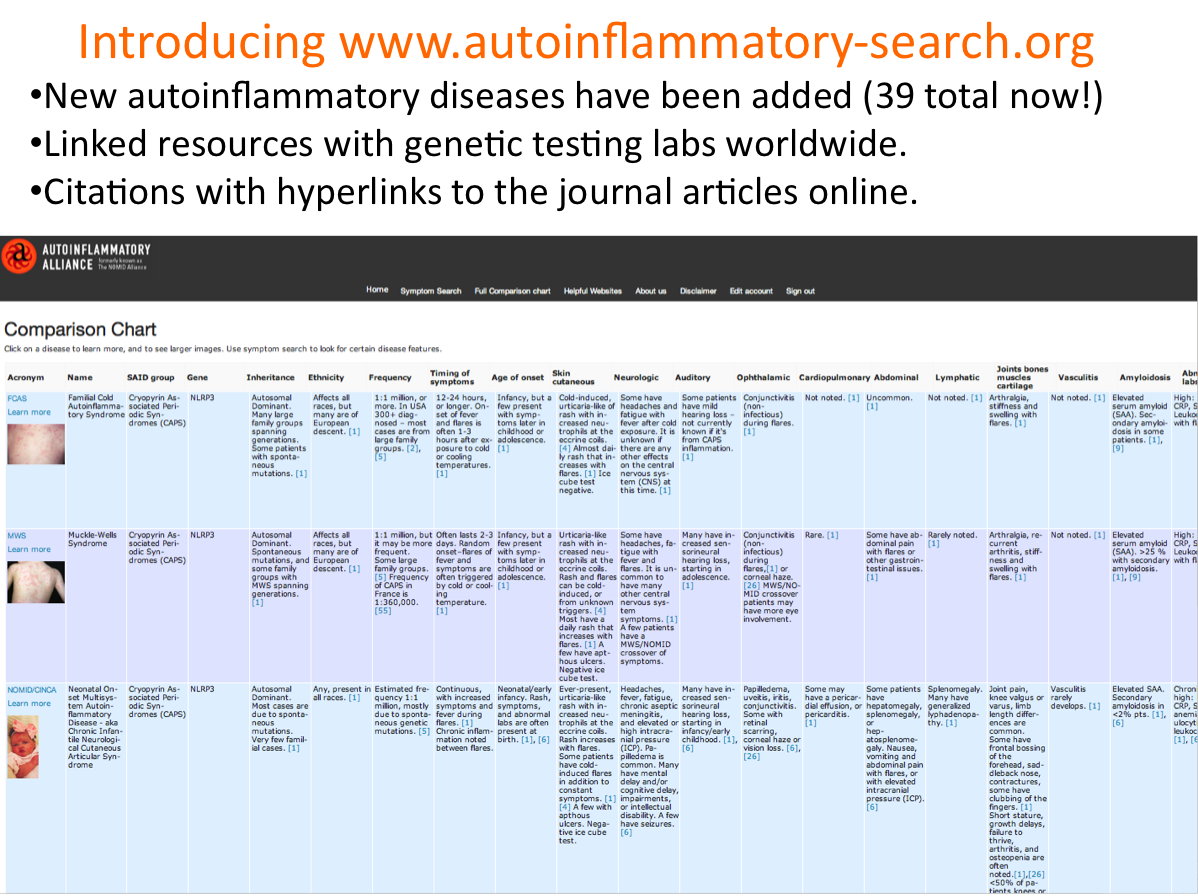
Autoinflammatory-Search.org -Chronic Nonbacterial Osteomyelitis (CNO): Chronic Recurrent Multifocal Osteomyelitis (CRMO); and Synovitis, Acne, Pustulosis, Hyperostosis, Osteitis Syndrome (SAPHO) – Symptoms and lab results for CRMO and SAPHO on the autoinflammatory database website.
Textbook of Pediatric Rhematology Autoinflammatory Bone Disorders Chapter – This was written by experts Dr. Polly Ferguson and Dr. Ronald Laxer. It has details on clinical symptoms, differencial diagnosis, and treatment for CRMO, Majeed syndrome, DIRA, and cherubism.
Chronic Recurrent Multifocal Osteomyelitis (CRMO) – This is one of the easiest to understand descriptions of CRMO. “Chronic recurrent multifocal osteomyelitis (CRMO) is an autoinflammatory (NOT autoimmune) disorder that mostly affects children. It comprises periodic bone pain, fever, and the appearance of multiple bone lesions that can occur in any skeletal site. The origin of this disease is unclear, but genetics appears to play a role. The clinical and radiological features on the disease are variable and the diagnosis can be difficult.”
Common symptoms include deep aching pain, limping, and fever. Other symptoms can include uveitis, IBD, psoriasis, acne, and pustules on the soles of the feet and palms of the hand. In some cases, Majeed syndrome is associated with CRMO. Other names for CRMO include SAPHO, chronic multifocal osteomyelitis, and chronic recurrent multifocal osteomyelitis.
CRMO Phenotypes Identified in Large French Cohort – Gives detailed information on 3 subgroups of CRMO patients, their disease progression and remission rates.
“In our cohort, after a mean disease duration of 4 years, only 74/171 (43%) of cases of CRMO were considered to be in clinical remission of which 40% were under treatment [while] among CRMO patients with active disease at the last medical visit, 71% remained on therapy [although] some of them had discontinued treatment,”
“These results suggest that CRMO may have a poorer prognosis than previously described with more frequently active disease at follow-up.”
Chronic recurrent multifocal osteomyelitis (CRMO) in children – single-centre clinical observations and experience.- Study of 42 children diagnosed with CRMO. Median age of onset was 10 to 11 years old. Most had bone pain as the first symptom. During flares, osteocalcin levels were high.
Unusual onset of a case of chronic recurrent multifocal osteomyelitis – “We report here a case a 12 years old girl with CRMO arising with recurrent episodes of left supraorbital headache, followed by the appearance of a periorbital dyschromia. Magnetic resonance imaging (MRI) of the skull and orbits revealed an important subacute inflammatory process. Few months after, the child presented a painful swelling of the left clavicle; the histological examination of the related biopsy allowed to establish the diagnosis of CRMO.”
Autoinflammatory bone disorders with special focus on chronic recurrent multifocal osteomyelitis (CRMO) – This is a review of autoinflammatory bone disorders including pyogenic arthritis, pyoderma gangrenosum and acne (PAPA), deficiency of IL-1 receptor antagonist (DIRA), Majeed syndrome, and CRMO. Symptoms, diagnosing, and treatment options are covered. From the article: “Autoinflammatory bone disorders are the result of a disturbed regulation of the innate immune system, resulting in immune cell infiltration of the bone and subsequent osteoclast differentiation and activation, osteolysis and bone remodeling. Though bone biopsies usually remain sterile, lesions mimic infectious osteomyelitis in histology and on radiographs [2-5]. Interestingly, autoinflammatory bone disorders are associated with inflammation of the skin (palmoplantar pustulosis, acne, psoriasis, Sweet syndrome) and/or the intestine (Crohn’s disease, ulcerative colitis, coeliac disease).”
“Furthermore, CNO can be part of the so-called SAPHO syndrome (Synovitis, acne, pustulosis, hyperostosis, and osteitis), which manifests in adolescence or adulthood. Whether CRMO in juvenile patients and SAPHO syndrome are the same disorder in different age groups remains to be determined.”
Chronic Recurrent Multifocal Osteomyelitis in Children: A Multidisciplinary Approach is needed to establish a Diagnosis. – This is a single case report of a 6-year-old girl diagnosed with CRMO. It goes into detail of her symptoms that included fever and swelling of her leg, blood test results, scans, and more. “This study clarifies the clinical and radiologic features of CRMO.”
Chronic recurrent multifocal osteomyelitis – Basic explanation of CRMO from ORPHA.net. Average age of onset is 10 years old. Bone inflammation can occur anywhere, but this notes that: “Metaphyses and epiphyses of the long bones are most frequently affected, in addition to the pelvis, the shoulder girdle and the spine.” Also noted, “Adult-onset forms are reported that resemble SAPHO syndrome. It is not clear whether SAPHO syndrome and CNO/CRMO are two separate entities or if they are part of the same disease spectrum with CNO/CRMO being the pediatric equivalent of SAPHO syndrome.” Most cases have periods of frequent flares and then remission and eventually resolve over time. In some, CRMO causes permanent bone deformities.
Whole-body magnetic resonance imaging: an essential tool for diagnosis and work up of non-oncological systemic diseases in children – “Twenty-one children underwent general anesthesia. WBMRI was a useful tool to provide correct diagnosis in chronic recurrent multifocal osteomyelitis (CRMO), and to identify the origin of fever or arthralgia of unknown etiology.”
Chronic recurrent multifocal osteomyelitis: case series of four patients treated with bisphosphonates – Case series of four patients with CRMO and treatment outcomes. No patients responded to NSAIDs. All were treated with either alendronate or pamidronate with good response. This induced clinical remission in 2 of the 4 patients.
Chronic recurrent multifocal osteomyelitis: typical patterns of bone involvement in whole-body bone scintigraphy. – This study involved performing whole-body magnetic resonance imaging on 53 patients with CRMO. The results show specific common characteristics of CRMO and shows that WB-MRI is an important tool in diagnosing CRMO. “Results: WB-MRI revealed multifocal lesions in all but one patients. Only 26 of them had presented with multifocal complaints. We detected 1 – 27 geographic lesions/patient (mean 9.7). 510 of 513 lesions were significantly hyperintense compared to normal bone marrow. The pelvis, lower extremities, shoulders and spine were most frequently involved. 40 patients (75 %) had bilateral symmetrical involvement of bones. Most of the lesions were located in tubular bones, in 87 % adjacent to one or both sides of a growth plate. 32 % of lesions showed periosteal involvement. Of 456 affected bones, 33 (7.2 %) were deformed, 6 (18 %) were vertebra plana. Conclusion: In the absence of more specific diagnostic criteria, WB-MRI can, in synopsis with clinical findings, substantially contribute to a rapid diagnosis of CRMO.”
Chronic recurrent multifocal osteomyelitis in a 13 year old female athlete: a case report. – In this case, a 13-year-old girl had ankle pain and a history of sore feet, various pains in knees, back, and shoulder along with headaches and sensitive skin. She did not have unexplained fevers. Her father also had a history of unexplained muscle and bone pain. This study includes many other details such as differential diagnosis, treatment options, and MRI pictures.
Diagnostic criteria from this study:
Iyer et al.12, have formulated systematic approach to assist in making the diagnosis of CRMO by exclusion using the following criteria:
- Lack of causative organism
- No abscess, fistula or sequestra formation
- Radiographic appearance of sub-acute or chronic osteomyelitis
- Atypical location compared to infectious osteomyelitis
- Non-specific histopathologic and laboratory findings compatible with sub-acute or chronic osteomyelitis or other known disease process
- Prolonged (> 6 months) and recurrent painful symptoms
- Accompanying pustulosis palmoplantaris or acne
The laboratory findings suggest an inflammatory process with evidence of elevated ESR, C-reactive protein and alkaline phosphatase in approximately two-thirds of cases. A tissue biopsy is commonly required in order to rule out more sinister diagnoses such as tumour or infection. Cultures of blood and bone, along with microbial laboratory assays are negative for infectious processes.
Also noted, “CRMO is widely believed to be a pediatric equivalent of SAPHO syndrome.”
Chronic recurrent multifocal osteomyelitis causing an acute scoliosis. – A case study of a 15-year-old girl who developed scoliosis secondary to CRMO.
Typical patterns of bone involvement in whole-body MRI of patients with chronic recurrent multifocal osteomyelitis (CRMO). – “In the absence of more specific diagnostic criteria, WB-MRI can, in synopsis with clinical findings, substantially contribute to a rapid diagnosis of CRMO.”
Chronic recurrent multifocal osteomyelitis. “Chronic recurrent multifocal osteomyelitis (CRMO) is an autoinflammatory bone disease occurring primarily in children and adolescents. Episodes of systemic inflammation occur due to immune dysregulation without autoantibodies, pathogens or antigen-specific T cells.”
Chronic non-bacterial osteomyelitis in childhood – a comprehensive review. “The clinical picture of childhood chronic recurrent multifocal osteomyelitis (CRMO) is characterized by an aseptic chronic osteomyelitis, most often affecting the metaphyses of the long bones. Skin inflammation (palmoplantar pustulosis, psoriatic lesions, acne) and inflammatory bowel disease may be associated with CRMO and therefore subsume this disease into the entity of SAPHO syndrome.”
Chronic recurrent multifocal osteomyelitis mimicking osteoid osteoma. A detailed case report of a 9-year-old girl diagnosed with CRMO. Includes testing done and radiograph images.
Schnitzler’s Disease as an Important Differential Diagnosis of Chronic Recurrent Multifocal Osteomyelitis: A Case Report – Schnitzler’s disease and CRMO can have similar symptoms. “CRMO and Schnitzler’s syndrome are diagnosed by exclusion. At first sight, both diseases can be similar in their manifestation. However, considering the patient as a whole, the age of onset, the male gender, and the very atypical pruritic urticarial lesions on the trunk led to the correct diagnosis. CRMO is associated with pustulosis palmoplantaris, whereas Schnitzler’s disease is associated with neutrophilic dermatitis.”
Current Understanding of the Pathogenesis and Management of Chronic Recurrent Multifocal Osteomyelitis – Detailed overview of CRMO including diagnosing, symptoms, treatment, and genetics. Majeed, DIRA, and SAPHO are discussed.
Spinal involvement in chronic recurrent multifocal osteomyelitis (CRMO) in childhood and effect of pamidronate. – This study looked at how many with CRMO had involvement of the spine. Of 102 children and teens, 27 had spine deformities, back pain, and/or spinal lesions. Pamidronte was determined to be effective with few side effects.
Chronic Recurrent Multifocal Osteomyelitis-The Prevalence of Lower-Limb and Foot Involvement -“This study presents one of the largest published cohorts of pediatric patients with CRMO and also presents racial/ethnic group data that have not previously been reported in other studies. Despite being a condition considered to affect the metaphysis of long bones, the ankle area and foot bones were also frequently affected.”
Parotid swelling and chronic recurrent multifocal osteomyelitis of mandible in children – “Parotid mass or swelling is a common presentation of CRMO involving the mandible.”
A proposed treatment scheme for chronic recurrent multifocal osteomyelitis (CRMO): a case series of nine patients – “Our treatment policy in CRMO is to start with NSAIDs and MTX. If the patient is refractory to these drugs, anti-TNF treatment is commenced. Anti-TNF treatment was effective in the treatment of our CRMO patients, We suggest that extending the dosing interval is an effective option once they are in remission for 6 months. We also suggest that imaging may be included as an outcome measure in patients with CRMO.”