Updated 2/15/2022
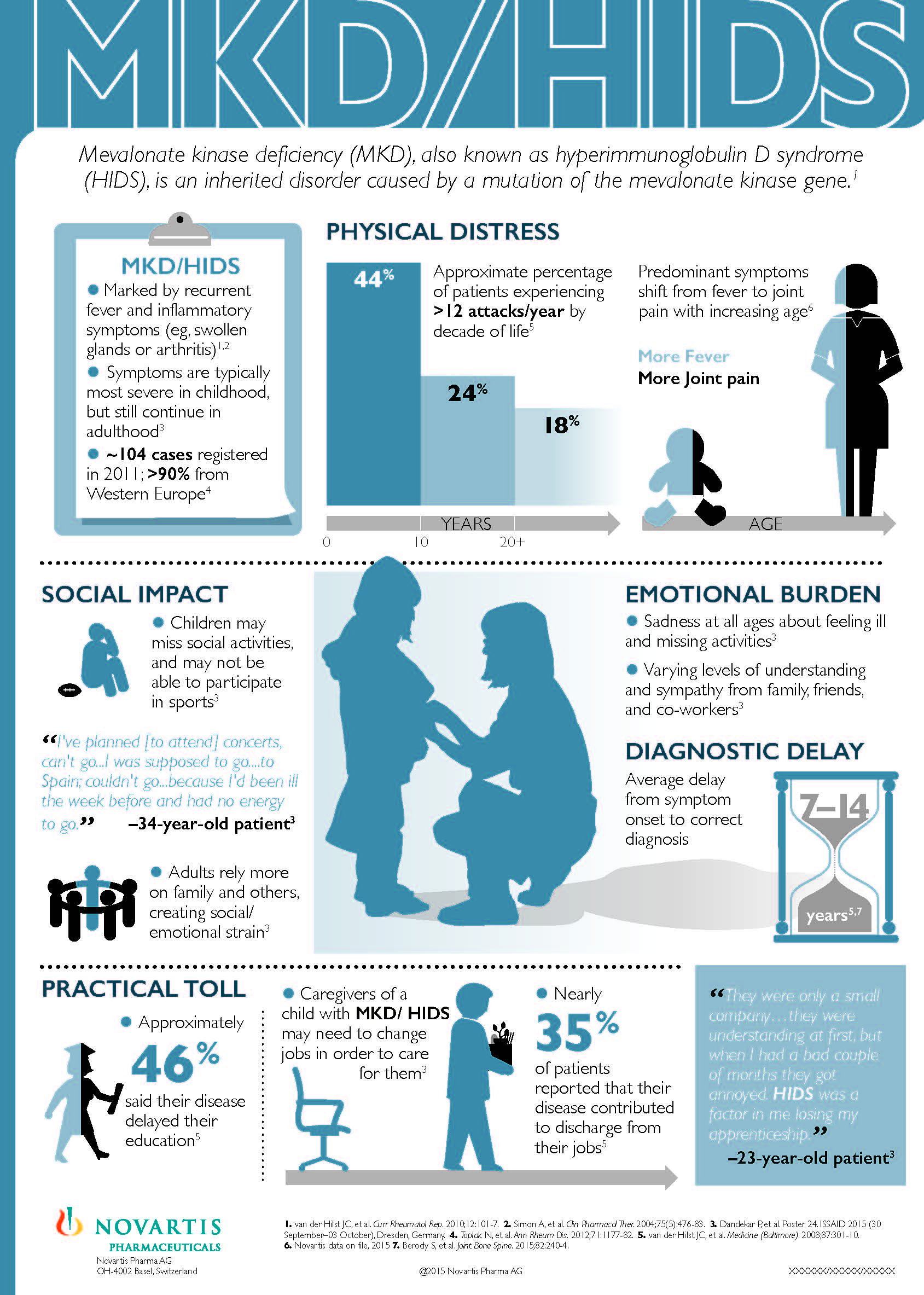
HIDS (hyper-IgD syndrome, a mevalonate kinase deficiency) and PFAPA (periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis) are both periodic fever syndromes that generally start in childhood and have very similar symptoms. It can be difficult to distinguish PFAPA from HIDS clinically. This is because the fever length, frequency, and main symptoms including mouth ulcers, pharyngitis, and swollen cervical lymph nodes occur in both HIDS and PFAPA. In fact, one study showed 83% of HIDS patients meet PFAPA diagnostic criteria.
However, unlike PFAPA, HIDS is a lifelong condition that comes with serious risks if not treated. Getting a correct diagnosis and treatment greatly reduces possible serious complications from HIDS.
Below is a comparison of symptoms, labs, and other details of PFAPA vs. HIDS. This chart illustrates why genetic testing is such an important tool in helping to diagnose a patient with a suspected periodic fever syndrome, such as HIDS or PFAPA.
PFAPA may not yet have a genetic test available, but it is still important to run these tests to help with the diagnosis. In Textbook of Autoinflammation published in 2019, Drs Ceccherini, Rusmini, and Arostegui state, “The importance of genetic tests to reach a definitive diagnosis has become evident during the past few years.” They also note that advancements in genetics, “has resulted in the increased awareness of the clinical diversity of these diseases, best therapeutic approaches and follow-up schemes for the patients…”
Did You Know?
| An uncomplicated tonsillectomy costs $4,000 to $7,000. |
| Cost of genetic testing for 207 immune deficiency and autoinflammatory genes: $250 at Invitae. |
Of all the periodic fever syndromes, HIDS and PFAPA can be the most easily confused. However, PFAPA can also overlap in symptoms with Behcet’s-like autoinflammatory syndrome (HA20), FMF, TRAPS, and CAPS.
- Click here to see the autoinflammatory disease comparison chart for more details.
- Click here to see PFAPA vs HIDS at autoinflammatory-search.org.
- The Eurofever Classification Criteria is a good resource in evaluating patients who have PFAPA symptoms. This diagnostic questionnaire by the EUROFEVER project is really helpful for doctors considering symptoms when trying to diagnose some of the hereditary periodic fever (autoinflammatory) syndromes, like CAPS, TRAPS, HIDS and FMF. CAPS, TRAPS, HIDS, and FMF all have symptoms similar to PFAPA.
Keep in mind that in HIDS and PFAPA, disease severity and symptom presentation varies among patients. Not every patient has every symptom.
PFAPA vs HIDS
| PFAPA | HIDS | |
|---|---|---|
| Symptoms | Fever accompanied by pharyngitis and at least one of the following symptoms for a diagnosis: mouth ulcers, and/or swollen neck lymph nodes. | Fever with several other inflammatory symptoms. These can include: mouth ulcers, pharyngitis, swollen lymph nodes, joint swelling and pain, abdominal pain, diarrhea, vomiting, headaches, enlarged liver, and/or enlarged spleen. Some patients have a rash with flares. |
| Some have headaches, nausea, and possibly joint pain. Rashes are not typical.** | Symptoms vary between individuals and between flares in the same individual. | |
| Do symptoms occur outside of the fever? | No | Sometimes in some patients. Some patients are completely healthy between flares. |
| Vaccine Reactions | None. Flares are cyclic and on a predictable schedule. | Most have flares within 24 hours after some or all vaccinations. |
| Age of Onset | Usually between 2 to 5 years old. Rarely before age 1. | Usually before age 1. Some adult onset cases reported, confirmed with genetic testing. |
| Prognosis | Most children outgrow PFAPA by age 10-11 or about 6 years after symptoms started. | Lifelong disease. Symptoms and flare frequency change throughout life and may decrease in adulthood. |
| Flare Frequency/Pattern | Average of once a month. Flares are cyclic and very predictable–some are predictable to the day. | Average of every 2 to 12 weeks in childhood. Some may have regular predictable flares occurring monthly and some flares may be erratic and unpredictable. Flares are often triggered by injury, illness, vacations, school, birthdays, etc. |
| Flare frequency may spread out as kids begin to outgrow PFAPA. | Flare patterns often change throughout life. | |
| Fever Length | Average 3 to 5 days. Rarely more than 7 days. No more than 10 days. | Average 3 to 7 days. May last 10 to 14 days. |
| Temperature Range | 102-104+ degrees F | 102-104+ degrees F |
| Response to Prednisone (Standard dosing starts at 1mg/kg for both PFAPA and HIDS.) | One study showed 94% of PFAPA patients have full resolution of fever and flare symptoms with one dose. Resolution of symptoms with a single dose of prednisone is part of the diagnostic criteria here. | Some HIDS patients have full resolution of fever and flare symptoms with one dose. |
| Some are given a second dose if the flare returns the next day. | Some need a second or third dose to resolve all symptoms. | |
| Use of prednisone may increase flare frequency for some but not all with PFAPA. | Use of prednisone may increase flare frequency for some but not all with HIDS. | |
| Effectiveness of prednisone may decrease over time in some patients. | ||
| Most Effective Treatments | Ibuprofen, prednisone, tonsillectomy. Off-label use of anakinra* and colchicine in some studies. | Prednisone, anakinra* (off-label), canakinumab. |
| Genetics | Possibly genetic, but no gene yet identified. Research shows there are many cases of PFAPA with a family history of recurrent fevers and tonsillectomy. | Genetic testing available for the MVK gene mutation. Most cases are autosomal recessive. However, some patients with HIDS disease have only one mutation found. |
| Blood Tests | High CRP, WBC, and ESR during fevers. | High CRP, WBC, and ESR during fevers. |
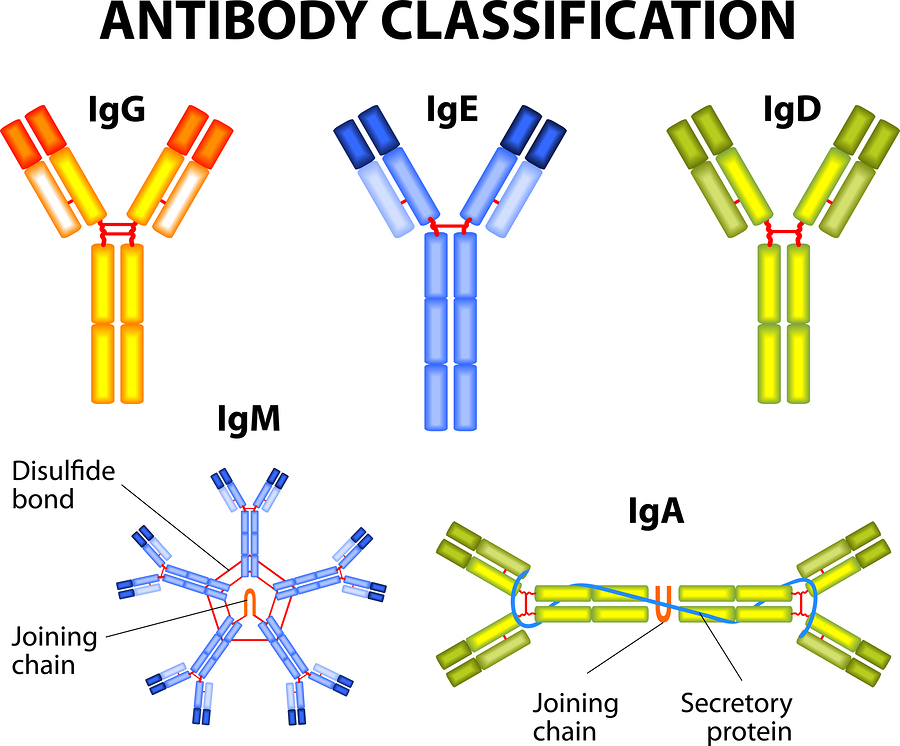
| Some have high IgD. | Some have high IgD, also accompanied by elevated IgA in up to 80% in some studies, but IgD may be normal in some patients. IgD may not be elevated in young children and infants. IgD is not to be the sole diagnostic test for HIDS. | |
| All blood tests will return to normal between flares. | In some, all blood tests will return to normal between flares. In others, blood tests will remain high between flares. There is a spectrum of severity, and chronic inflammation within the diagnosis of HIDS. | |
| Diagnosis | Clinical only, which includes ruling out similar conditions such as HA20, FMF, CAPS, TRAPS, and HIDS with genetic testing and comparison of symptoms. | Genetic testing available for the MVK gene. Most cases are autosomal recessive. However, some patients with HIDS have only one mutation found. |
| Risk of Severe Complications | None. | Amyloidosis, Henoch-Schonlein pupura (HSP), respiratory infections, and macrophage activation syndrome have been reported. Some patients have enlarged liver and/or spleen and gastrointestinal issues. |
*These are not FDA approved treatments for HIDS or PFAPA.
**Dr. Beata Wolska-Kusnierz states here that usually there are no skin changes in PFAPA and if there is a rash, “autoinflammatory illnesses other than PFAPA should be considered in the diagnostic process.”
**In this study, patients met the study definition of PFAPA only “if they did not have arthritis or a distinctive rash or documented neutropenia.”
**UpToDate Periodic fever with aphthous stomatitis, pharyngitis and adenitis (PFAPA syndrome) authors state, “The following symptoms as a part of most attacks should trigger consideration of other diagnoses: cough, coryza, severe abdominal pain, significant diarrhea, rash, arthritis, or neuromuscular symptoms.”
Why is it important to differentiate between PFAPA, HIDS, and other periodic fever syndromes?
Although PFAPA is known to be outgrown by the teen years and causes no long-term health consequences, HIDS and other autoinflammatory diseases if left untreated can have serious risks and complications throughout life. Since there are specific treatments that benefit HIDS and other autoinflammatory diseases, and those treatments can be different for each condition, the right diagnosis that leads to early treatment can make a big difference in the life of the patient. A common treatment for PFAPA is a tonsillectomy, which is painful, and all surgery has risks. For HIDS, T&A is not a highly effective treatment, and surgeries can trigger severe flares for a patient with HIDS who is not on effective treatment. It’s best to determine if a patient has PFAPA, and not some other periodic fever syndrome prior to surgery.
Genetic testing as part of the autoinflammatory diagnosis will help determine if a patient has another autoinflammatory disease such as HIDS.
Genetic Testing is Easy to Do and Inexpensive
However, a number of doctors treat patients with periodic fever symptoms as having PFAPA before exploring other fever syndromes. They only pursue genetic testing or other tests for known autoinflammatory diseases after a patient fails to have a reduction, or remission of symptoms after having a tonsillectomy, or they continue to have symptoms into their teenage years, or older. Some doctors cite challenges in getting insurance approval for genetic testing, or are concerned about if the insurance will consider the testing unnecessary if the results are negative for other autoinflammatory diseases. The cost for the genetic testing is less than a tonsillectomy, and now there are several laboratories doing the testing at inexpensive prices, so it is easier to get insurance approval. (More info on labs to use for the testing here.) Having a negative result on the genetic testing for other periodic fever syndromes actually would help to support the PFAPA diagnosis, if the patient also met the diagnostic criteria for PFAPA, so it is not a “wasted expense” for the test.
Genetic Testing is One Diagnostic Tool
It is also important to keep in mind that genetic testing is just one tool in the diagnostic process. Several factors need to be considered in diagnosing any autoinflammatory disease, including both PFAPA and HIDS. These include collectively looking at symptoms, age of onset, blood test results, and genetic testing results. Patients with PFAPA do not have signs of chronic inflammation, or elevated inflammatory markers when not having flares of symptoms, so testing patients during a flare, and when they are not flaring is helpful. Some autoinflammatory diseases can have signs of chronic inflammation between flares of fevers and more notable symptoms, so it is important to do a series of lab tests over a few weeks to get a bigger picture of what is going on.
Research is Ongoing
Every year new autoinflammatory genes are discovered. Until science can catch up to patients, for some patients a clinical diagnosis is best even if genetic testing was negative.
There are patients with various autoinflammatory diseases that may clinically be diagnosed and respond to the suggested treatments for a certain genetic disease even though they do not have a genetic mutation found for that disease. So, having a genetic testing result with no mutations, but the patient fits the criteria for a certain disease should not rule out having that specific disease. New advances in genetics are finding mutations for some of these diseases (especially CAPS) that were not found previously with the standard genetic testing process.
If you are having difficulty getting the genetic fever panel test done, here are some resources that can help:
The Autoinflammatory Alliance is a 501(c)(3) non-profit organization dedicated to helping those with autoinflammatory diseases.
Donate now to help with awareness, education, and research for these rare diseases.
References
- ACTA Paediatrica: A clinical review of 105 patients with PFAPA (a periodic fever syndrome)
- Children’s Mercy Kansas City: Diagnosing PFAPA in your clinical practice
- Nature Reviews Rheumatology: Clinical features and management of CAPS and PFAPA Table 2
- Healio: A 2-Year-Old Patient Has Had Recurrent Fevers For The Last Year. He Often Has A Red Throat, Adenopathy, And Stomatitis With His Fevers. I Am Concerned About Periodic Fever, Aphthous Stomatitis, Pharyngitis And Cervical Adenitis Syndrome. What Are The Treatment Options For This Diagnosis?
- PubMed.gov: PFAPA syndrome: clinical characteristics and treatment outcomes in a large single-centre cohort.
- Pediatrics: Differentiating PFAPA Syndrome from Monogenic Periodic Fevers
- PubMed.gov: Elevated immunoglobulin D levels in children with PFAPA syndrome.
- PubMed.gov: First report of macrophage activation syndrome in hyperimmunoglobulinemia D
- Pediatrics: Mevalonate Kinase Deficiency: A Survey of 50 Patients
- SAID Support: Hyper-IgD Syndrome
- DermNet NZ: Hyperimmunoglobulinaemia D with periodic fever syndrome
- Cost Evaluation: How Much Does a Tonsillectomy Cost?
- To Make The PFAPA Syndrome More Familiar by Dr. Beata Wolska-Kusnierz
- BMJ: Recommendations for the management of autoinflammatory diseases
- UpToDate Periodic fever with aphthous stomatitis, pharyngitis and adenitis (PFAPA syndrome)