Since 1994, researchers at the National Institutes of Health in Bethesda, MD near Washington D.C., have been studying various periodic fever syndromes and providing care and treatment to thousands of patients with these rare conditions. Through two main studies, patients with CAPS (NOMID, FCAS, and MWS), FMF, TRAPS, HIDS, PFAPA, DIRA, Behçet’s, CANDLE syndrome, PLAID, DADA2 plus other similar rare diseases, and undiagnosed autoinflammatory syndromes receive help understanding and treating their condition. Through these studies great advancements have been made in the last 20+ years. Thanks to the researchers and patients in the studies, getting a diagnosis has become easier and more accurate with genetic tests, treatments have been developed, and a greater overall understanding of these conditions has been gained.
The researchers at the NIH are some of the leading autoinflammatory experts in the U.S. and around the world. Through the NIH, patients throughout the U.S. and in some cases the world who otherwise do not have local doctors with experience in their condition, can get ongoing expert care and individual treatment plans. For many, NIH care has been lifesaving.
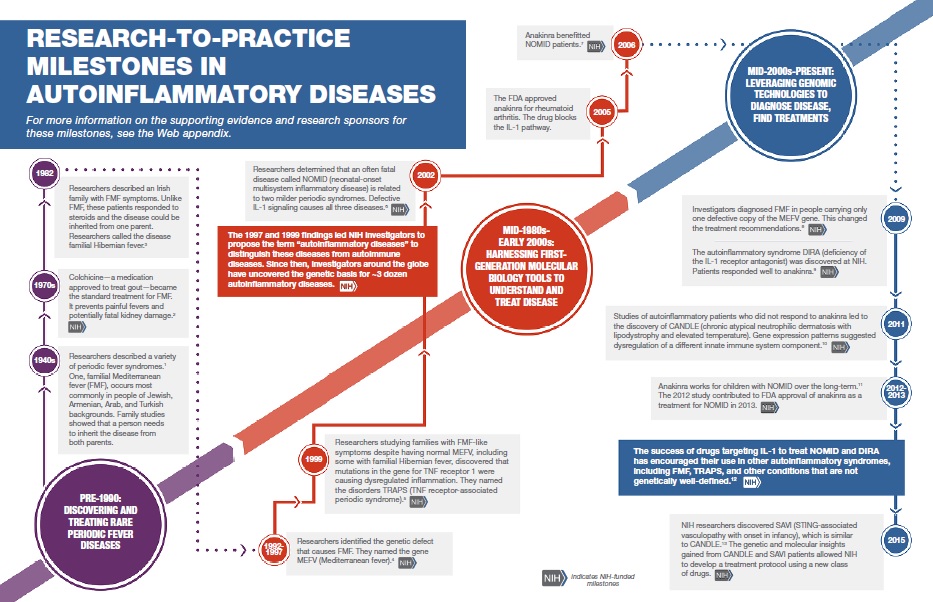
Click here to see the history of autoinflammatory disease research at the NIH.
About the Two Main Autoinflammatory Studies
Although dozens of studies have been published by the NIH in relation to autoinflammatory disease, there are two main protocols from which most of these study participants were first enrolled in at the clinical center. Both studies are called “natural history” studies. This is where researchers follow patients to learn about the disease and provide help with understanding their condition and with treatment plans. The researchers heading these studies collaborate to help patients and for research.
Familial Mediterranean Fever and Related Disorders: Genetics and Disease Characteristics
This is the longest study of these conditions. It is led by Dr. Daniel Kastner who led the teams that discovered both the FMF gene and TRAPS gene. Dr. Kastner is also director of the NIH’s National Human Genome Research Institute. This study accepts, “patients with known or suspected familial Mediterranean fever, TRAPS, hyper-IgD syndrome or related disorders.” (Click here for the study details.) As of 2012, there were about 1900 patients in this study with the following breakdown:
- No mutation found/undifferentiated – 66%
- FMF – 21%
- TRAPS – 6%
- CAPS – 4%
- HIDS – 1%
- DIRA – 1%
- Polygenic – 1%
- Crohn’s Disease, PAPA, and Blau Syndrome – 0% (a handful of patients)
Natural History, Pathogenesis, and Outcome of Autoinflammatory Diseases (NOMID/CAPS, DIRA, CANDLE, Still’s-like Diseases, and Other Undifferentiated Autoinflammatory Diseases)
This study is led by Dr. Raphaela T. Goldbach-Mansky. Dr. Goldbach-Mansky and her team have helped discover new diseases such as DIRA, and discovered the biological processes involved in NOMID, which has led to successful treatment for many patients. This study accepts patients “with known NOMID/CAPS, DIRA, CANDLE, SAVI, NLRC4-MAS, Still’s Disease, and with other yet undifferentiated autoinflammatory diseases.” Click here for more details on this study.
Who has the NIH helped?
To get a peek into the amazing research done by the NIH and how they have directly helped patients read:
Meet Alex Before and After NIH Clinical Trial here
What are the Costs to Patients?
The NIH is federally funded by taxpayers. (Read more here about how NIH research funding benefits everyone.) Once accepted into the study, and as of 2017, all treatment and care provided by the NIH is free to patients.
Children and their families can stay at the Children’s Inn for free, which is conveniently located directly across from the NIH. The Children’s Inn provides a comfortable child and teen-friendly home away from home for all kids needing treatment at the NIH.
For adult patients, accommodations can be made at local hotels for a reduced cost.
Depending on the study and current budget, flights may also be available for free or at a reduced cost.
Once patients are back at home, the NIH researchers will continue to consult with the patient’s local doctors as needed and can even help with providing documentation to insurance companies to help gain approval for recommended treatments not provided through the study.
Take a Virtual Tour of the Children’s Inn at the NIH
How to Join a Study and Get Help
You do not necessarily need a doctor to refer you or to set up admission into the study. If you or your doctors think you or your child has a periodic fever syndrome, then you can call the appropriate department yourself to be screened for inclusion in the study. You will need to submit medical records and doctor statements pertaining to yours or your child’s fever illness, but you can call first to get the process started and get more information on what is needed. Once the team has received your records, they will evaluate them to determine if you meet the criteria for inclusion in the study.
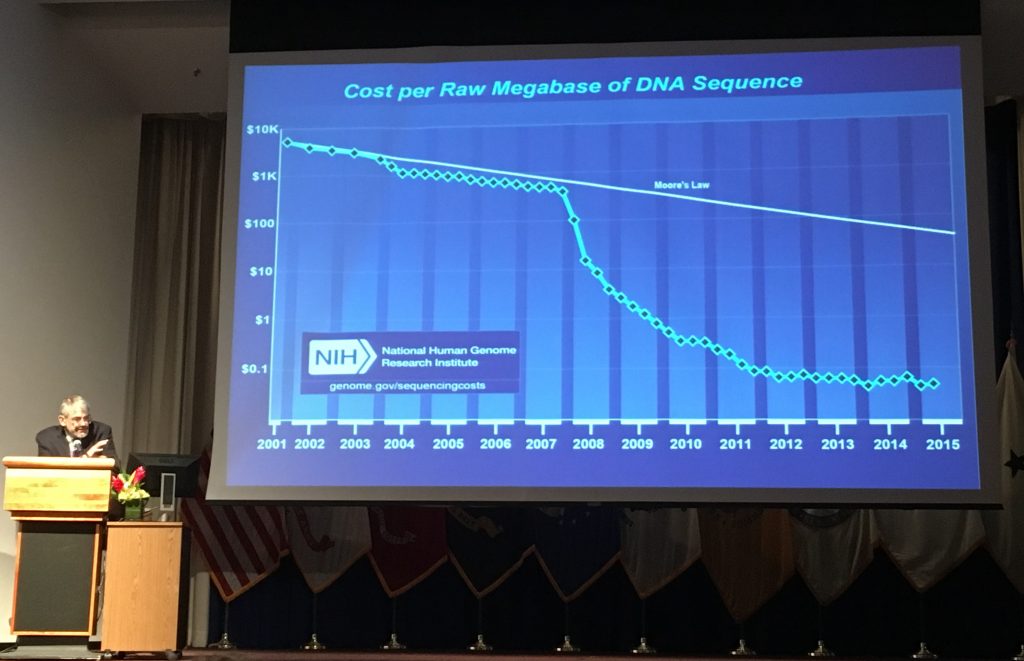
Dr. Kastner of the NIH speaks at the first Autoinflammation & Immune-dysregulation Symposium in 2016 about the decreasing costs of genetic testing, and the importance of genetic research and testing in autoinflammatory diseases. Click here to read more.
Even if your genetic tests results were negative for any known periodic fever mutation, you may still qualify for one of these studies if you have symptoms of a fever syndrome. In the Familial Mediterranean Fever and Related Disorders: Genetics and Disease Characteristics study, about 2/3 of the patients do not have a known or identifiable mutation. One of the many study goals is to identify new genes involved which will eventually lead to better treatments.
If you have a positive genetic test or are suspected of having FMF, TRAPS, HIDS or similar autoinflammatory disorder, then you or your doctor can contact Dr. Kastner’s team at (301) 402-2023. Click here for more information on this study.
If you have a positive genetic test or are suspected of having a CAPS disease, DIRA, CANDLE, Still’s-like disease, other related or unknown autoinflammatory disorder, then you can contact Dr. Goldbach-Mansky at (301) 402-7326. Click here for more information on this study.
Not sure of your diagnosis? That’s OK too. If you have symptoms of a periodic fever syndrome you can call either or both teams. The researchers will evaluate your medical records to determine if you fit in either protocol.
The following video features two of Dr. Kastner’s team and gives a good overview of the research they do and what goes on behind the scenes.
Other NIH Autoinflammatory Studies
Patients may be enrolled in more than one clinical trial for their disease, (but only one drug trial at a time). You can be in a clinical drug trial, and a natural history study concurrently.
CANDLE syndrome has a special compassionate use clinical drug trial with the drug, Baricitinib at the NIH. (This clinical trial also is designed to treat severe juvenile dermatomyositis (JDM), a different disease. )
The Undiagnosed Diseases Program (UDP) at the NIH has also been a key resource in new discoveries with many diseases, including autoinflammatory diseases. This is another option to consider, when seeking a diagnosis, but most cases that appear to be autoinflammatory are usually referred to the other main autoinflammatory disease studies under the Kastner Group, the Goldbach-Mansky Group, and/or the Translational Autoinflammatory Disease Section, also headed by Dr Goldbach-Mansky.
Click this link to see all the studies that are going on in the NIAMS division at the NIH, as they are ever-expanding their research into autoinflammatory diseases. Scroll down to the area featuring clinical trials for “Periodic Fever Syndromes and Other Autoinflammatory Diseases.”
Other Autoinflammatory Disease Studies
These are the main ongoing studies for autoinflammatory diseases in the U.S., but they are not the only autoinflammatory studies available to patients around the world. Search ClincialTrials.gov for more studies in the U.S. and around the world or contact the Autoinflammatory Alliance for information about other studies currently accepting new patients.
Adventures in the Genomics of Inflammation – Lecture by NIH Autoinflammatory Researcher Dr. Daniel Kastner
References
- ClinicalTrials.gov: Familial Mediterranean Fever and Related Disorders: Genetics and Disease Characteristics
- ClinicalTrials.gov: Studies of the Natural History and Pathogenesis and Outcome of Neonatal Onset Multisystem Inflammatory Disease (NOMID/CAPS, DIRA, CRMO, Still s Disease, Behcet s Disease, and Other Undifferentiated Autoinflammatory Diseases)
- Adventures in the Genomics of Inflammation – Daniel Kastner
- National Human Genome Research Institute: Raphaela Goldbach-Mansky, M.D.
- National Human Genome Research Institute: Dan Kastner, M.D., Ph.D.
- The Children’s Inn at NIH
- National Institutes of Health
- Translational Autoinflammatory Disease Section works in partnership with Dr. Dan Kastner the Adjunct Investigator of NIAMS, and his laboratory group.
- Compassionate Use Protocol for the Treatment of Autoinflammatory Syndromes (CANDLE syndrome study)
- Rilonacept for Deficiency of the Interleukin-1 Receptor Antagonist (DIRA)
- A Pilot Study of Anakinra in Behcet‘s Disease (BD)
- A Long-Term Outcome Study with the IL-1 Receptor Antagonist anakinra/Kineret in Patients with Neonatal Onset Multisystem Inflammatory Disease (NOMID/CINCA Syndrome) A Therapeutic Approach to Study the Pathogenesis of this Disease