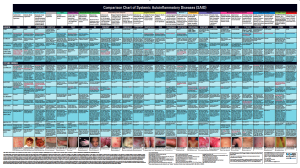
 The Autoinflammatory Alliance’s Comparison Chart of Systemic Autoinflammatory Diseases had it’s debut in the poster presentations at the 7th Congress of ISSAID 2013 in Lausanne, Switzerland to medical professionals from around the world. It was edited, and expanded for release in larger distribution at the American College of Rheumatology 2013 Meeting in San Diego, CA in October 2013, and is available in print, or online. We are working on developing an interactive, multi-lingual digital format for release in 2014. The content was written, and edited by the leading experts on autoinflammatory diseases worldwide and was co-authored by Karen Durrant, RN BSN–President of the Autoinflammatory Alliance (formerly The NOMID Alliance).
The Autoinflammatory Alliance’s Comparison Chart of Systemic Autoinflammatory Diseases had it’s debut in the poster presentations at the 7th Congress of ISSAID 2013 in Lausanne, Switzerland to medical professionals from around the world. It was edited, and expanded for release in larger distribution at the American College of Rheumatology 2013 Meeting in San Diego, CA in October 2013, and is available in print, or online. We are working on developing an interactive, multi-lingual digital format for release in 2014. The content was written, and edited by the leading experts on autoinflammatory diseases worldwide and was co-authored by Karen Durrant, RN BSN–President of the Autoinflammatory Alliance (formerly The NOMID Alliance).
We have narrowed the focus of the chart to Systemic Autoinflammatory Diseases (SAID), because these share some similar characteristics, yet unique findings between them, and can be very hard to distringuish from each other.
Some Main features of Systemic Autoinflammatory Diseases (SAIDs) include:
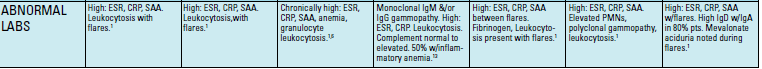
- Most have known genetic mutation (or in a few cases, deletions) that cause the disease, so the right genetic testing could help with diagnosis. However, there are some patients that have the clinical findings, but may not show the genetic mutation, and respond to the appropriate treatment, so clinical diagnosis, based on symptoms, labs and other tests is the most important focus. This chart allows doctors to analyze the clinical symptoms, in addition to the common lab findings and genetic mutations associated with each disease.
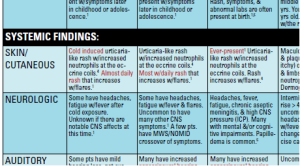
- The majority of SAIDs feature recurrent (periodic) fevers, along with other systemic symptoms (often rashes are present in most of these diseases) during flares.
- SAIDs are generally lifelong diseases, and in most cases they present in infancy or early childhood, and last throughout a patient’s lifetime. There are few adult-onset autoinflammatory diseases, and some patients that may have periods of remission, or lessened frequency of symptoms at various times in their life (and a few with PFAPA may even outgrow their condition), but in general, these are significant diseases that affect patients throughout their lifespan.
With this chart you can narrow down the possible systemic autoinflammatory diseases a patient might have and focus on what further testing is needed and best treatments to try first.
You can search symptoms on the chart by accessing the pdf, and then clicking the “command” and “F” key on your computer to bring up a small green search bar on the top of the pdf. Use the page tools to scroll through each area that has that word in your search.
Note-most of the symptoms on this chart are in medical terms, so you will need to use the medical (latin) name for a certain symptom (such as “conjunctivitis” instead of the common term “red eyes.”)
Basic Steps in Using the SAID Diagnostic Chart
- Read each symptom box on the chart.
- Circle the boxes with symptoms that you know the patient does have.
- Cross off what you are sure the patient does not have.
- If you do not know if the patient has a symptom, leave that box blank. In some cases, it may be appropriate to cross off some symptoms in a box and circle others in that same box.
- Then see which ones have the most circles and fewest symptoms or boxes crosses off. Those are the autoinflammatory diseases that warrant further investigation.
- Most patients will have symptoms that match more than one fever syndrome as many of these conditions share the same symptoms.
Evaluate the Patient Holistically to Obtain a Good Diagnosis
- The collections of symptoms need to be evaluated as a whole.
- Rarely does only one symptom or test give you the answer. Some symptoms do bear more weight and can help narrow down the possibilities.
- Fever pattern and length of fevers is a prominent symptom to consider. For example, most PFAPA fevers do not last longer than 6 days. If a fever has lasted more than 10 days, PFAPA and FMF may be pushed down on the list of possibilities, but kept on the list because there are always exceptions.
- The type of rash as identified by a dermatologist is also very helpful. Skin biopsies can lead to a more defined diagnosis with many of these diseases.
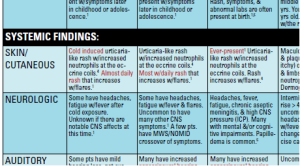 Other Key Considerations in Using this Chart:
Other Key Considerations in Using this Chart:
- Patients do not have to have every symptom on the list for a specific fever syndrome to have that syndrome.
- Patients may have additional symptoms not covered on the chart.
- Patients themselves, and caregivers of patients with suspected fever syndromes should also carefully read this chart, and discuss what symptoms they have from the chart with their doctor, as they know their own individual symptoms best.
- Not every patient presents a typical disease progression or has textbook genetic findings or other lab results.
- There are always exceptions, and there are still more unclassified conditions that will need to be added to this chart, so just because someone does not “fit” all the areas on this chart, they may still have an Undifferentiated (Unclassified) Autoinflammatory Disease, and should be cared for in the proper manner.
Keep in mind that not everyone gets every symptom on the list or has every symptom with every flare. Sometimes symptoms develop later in life. Some symptoms fade away while new ones develop. Some symptoms may have been easily missed or dismissed in infancy or early childhood when symptoms, such as rashes and fevers, are not considered unusual. Not having a certain symptom, doesn’t necessarily exclude that disease. To work towards a good diagnosis, the patient’s entire symptom or potential symptom history throughout their life needs evaluation.
For example, if the patient has never had a rash, you can cross of the rash symptom in every autoinflammatory disease. However, that does not mean that all of these diseases have now been ruled out. It only means rash is not a prominent symptom for that patient and the other symptoms need more weight.
Diarrhea is another common symptom in many fever syndromes. However, not having diarrhea during a flare does not mean it is not a fever syndrome.
Even a lack of fever does not exclude the periodic fever syndromes as a possibility. There have even been rare cases of patients with confirmed periodic fever syndromes not having the typical periodic high fevers. Familial Mediterranean Fever (FMF) can very rarely start with amyloidosis as the primary symptom rather than fevers. There are also reported cases of Tumor Necrosis Factor (TNF) receptor associated periodic syndrome (TRAPS) presenting without fever. Some of this variance can be due to the various genetics. In a few cases, some patients have somatic mosiacism, so not all their body tissues have the mutation, only some of them, which leads to an altered presentation of their disease. A good diagnosis takes careful evaluation of all the symptoms and lab tests as a whole.
 Now What?
Now What?
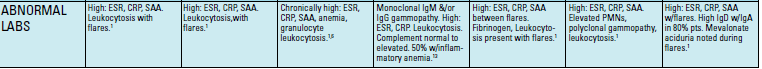
By now you should have a diagnostic chart that is well-marked with circles, X’s, question marks, and other notes. Look at the abnormal lab tests and genetic tests available for the diseases that are now high on the list of possibilities and determine if any of those tests still need to be done. Consider genetic testing for those conditions with the most circles and for conditions that have very similar symptoms. If your patient is in the U.S., The GeneDx 7-gene Periodic Fever Syndromes Panel is a good test to start with because it tests for 7 different fever syndromes that can look alike symptom-wise. This test only includes these genes: ELANE (ELA2), LPIN2, MEFV, MVK, NLRP3 (CIAS1), PSTPIP1, TNFRSF1A–which will allow for testing for FMF, TRAPS, CAPS (all 3 forms), HIDS & MA (both MVK diseases), PAPA, Majeed, and Cyclic Neutropenia (not on the chart because it is not considered in the same grouping as the other SAIDs). As of 2014, ARUP Laboratories also has a periodic fever panel genetic test available.
However, if your patient does not have characteristics for those diseases on that panel, but other conditions on the chart, you will need to send samples to be tested at another facility. One of the best resources to finding the right genetic testing facility for each disease is the GTR: Genetic Testing Registry which also lists the genetic labs worldwide. Other genetic and specialized tests available only at research facilities, such as the National Institutes of Health, may also be necessary. All these labs are on this registry, which is updated frequently.
For some diseases, such as FMF, there are many labs that can do the testing, but you do need to consider the type of test offered, and if it is the most comprehensive, since some labs may not test all the possible options for this mutation, but focus on the “most common” mutations. Look for the labs on the Genetic Testing Registry list for each disease that offers “Sequence analysis of the entire coding region.” Getting the right test is essential, so nothing is missed with the test, since they can be expensive and difficult to get approval for with insurance.
If PFAPA is a possibility, other hereditary conditions should be ruled out as part of the diagnosis, in part with the GeneDx or ARUP Laboratories fever panel. Studies have shown that 83% of patients with HIDS, 57% with TRAPS, and 8% with FMF meet the diagnostic criteria for PFAPA.
This chart was created by request of many doctors and researchers, and has quickly become an important diagnostic tool for rheumatologists, immunologists, patients, and parents of patients around the world. We have shared thousands of copies of it in print, and countless numbers have downloaded it online for reference. Our goal was to have a reference, with an easy to use comparison of symptoms, so medical professionals could consider these diseases when they were caring for patients with signs of autoinflammatory diseases.
 How to Print the Autoinflammatory Diseases Diagnostic Chart on Your Home Computer
How to Print the Autoinflammatory Diseases Diagnostic Chart on Your Home Computer
The full size Comparison Chart of Systemic Autoinflammatory Diseases (SAID) published by the Autoinflammatory Alliance is a very large poster. In PDF format if you just hit print you will need a magnifying glass to read it. Here’s how to print it full poster size on your computer.
You will need to have the latest Adobe Reader software installed on your computer.
Open the chart by clicking “Click here to download the disease comparison chart” from this page – http://www.autoinflammatory.org/compchart.php
Click the rectangular button with the arrow in it on the top right of your screen.
Choose “open with adobe reader.”
You can now highlight and even post notes on the chart with the yellow tools you see at the top menu bar. Zoom in to read it more clearly.
To print, click the printer button and choose “poster.” It will now print the entire poster full size on several pieces of paper. You will need to tape it together, but you won’t need a magnifying glass to read it.
Another option is to get an electronic copy to a local Kinko’s or other copy store and have them print it as a full size poster.
References
- GeneReviews: Familial Mediterranean Fever
- Annals of the Rheumatic Diseases: “Periodic fever” without fever: two cases of non‐febrile TRAPS with mutations in the TNFRSF1A gene presenting with episodes of inflammation or monosymptomatic amyloidosis
- Pediatrics: Differentiating PFAPA Syndrome From Monogenic Periodic Fevers
- GTR: Genetics Testing Registry
- GeneDX Periodic Fever Syndromes Panel (7 genes)
- Comparison Chart of Systemic Autoinflammatory Diseases
*Printer photo by morganlstudios/Bigstockphoto.com
 We are very excited to share our newest publication, the “Healthier Ever After” book to help families with young children thrive and cope with frequent (and often very painful) injectable medications to help treat autoinflammatory diseases.
We are very excited to share our newest publication, the “Healthier Ever After” book to help families with young children thrive and cope with frequent (and often very painful) injectable medications to help treat autoinflammatory diseases. One of the key features of the book is a guide to discuss various things related to their injection, so you can help develop a custom injection plan for your child.
One of the key features of the book is a guide to discuss various things related to their injection, so you can help develop a custom injection plan for your child. Click here to download a copy.
Click here to download a copy.