COVID-19 (coronavirus) is on the minds of many around the world, and in some regions, it has hit very hard. We know our autoinflammatory/periodic fever syndrome patient community is very concerned.
Below is a list of trusted resources and studies regarding autoinflammatory disease management with COVID19.
*If you have complex, chronic medical issues, or have any medical
concerns, consult with your doctors and medical professionals that care for
you or your loved ones on the proper disease management and infection
prevention for your family.*
*Please follow the WHO and CDC recommendations, and follow your local
and state guidelines for your part of the world.*
Management of childhood-onset autoinflammatory diseases during the COVID-19 pandemic – Rheumatology International July 2020
Patients ages 1 to 23 included FMF, PFAPA, CAPS, CRMO, DADA2, Blau, TRAPS, and HIDS. Treatments included colchicine, Ilaris, Enbrel, Kineret, Actemra, and Humira. Below are some highlights only from the study. To see the full study will all the information from the study click the link above to read the study in full.
“Among patients on biologic drugs, neither a symptom nor a positive polymerase chain reaction test for COVID 19 was detected. In conclusion, pediatric patients with AIDs, those receiving biologic treatment and/or colchicine, may not be at increased risk for neither being infected nor the severe disease course.”
“Given the immunosuppressive effects of biologic treatment and highly contagious nature of SARS CoV-2, it was interesting that these two patients who were receiving biologic treatment and had close contact histories were completely asymptomatic, with negative PCR tests.”
“Although serious concerns for patients on immunosuppressive treatment seems reasonable at first, there is no sufficient data in the literature supporting such an attitude.”
“Our preliminary experience shows that pediatric patients with AIDs, even if they receive biologic treatment, are not at increased risk for neither being infected with SARS CoV-2 nor the severe disease course. There are some recently published data suggesting protective role of biological treatments and colchicine on COVID 19. Moreover, autoinflammatory conditions such as FMF possible protects COVID 19 patients from the poor outcome. Bearing on mind the increased risk for disease flares during the infections among AID patients, we, rheumatologists, should warn our patients not to withdraw their medication, unless they are advised to do so.”
International Society of Systemic Auto-Inflammatory Diseases (ISSAID) Recommendations for COVID-19
Key recommendations for the care of autoinflammatory patients:
“3. At the moment for all patients with autoinflammatory diseases on medication, we recommend to continue all therapies as usual.
4. Don’t stop your medications including colchicine and biologics, without consulting your doctor. This may cause a flare of your autoinflammatory disease.
5. If you are on corticosteroid therapy – consult your doctor regarding possible dose adjustment.
6. Patients in isolation or quarantine (without symptoms) should continue therapy as usual.
7. In case of fever and suspicion of infectious diseases follow your national advice for access to health care and to test for Covid-19. In the meantime, continue colchicine and, if taking biologics, get in touch with your treating physician for guidance.”
(adapted from the EULAR recommendations)
“Ongoing treatment of patients with PRD and probable or confirmed symptomatic COVID-19 infection:
• NSAIDs, HCQ and colchicine may be continued, if necessary, to control underlying disease (H).
• IL-1 and IL-6 inhibitors may be continued, if necessary, to control underlying disease (H).
• Glucocorticoids should be continued, with an effort to reduce the dose to the lowest dose possible to control underlying disease and avoid adrenal insufficiency (H).”
COVID-19 Global Rheumatology Registry
“In response to the evolving global COVID-19 coronavirus pandemic, we are
creating a secure, de-identified, international case reporting registry. It is
our hope that the information collected will help guide rheumatology clinicians in assessing and treating patients with rheumatologic disease and in evaluating the risk of infection in patients on immunosuppression.”
Please share this registry with your rheumatologist or immunologist so the
doctor can submit a case report. http://rheum-covid.org/
Paediatric Rheumatology European Association (PReS) Recommendations for Coronavirus Outbreak
“3. At the moment for children with rheumatic diseases on medication, we recommend to continue all therapies as usual.
- Don’t stop your medications including methotrexate (MTX) and biologics, without consulting your rheumatologist. This may cause a flare of your rheumatic disease.
- If you are on corticosteroid therapy – consult your rheumatologist regarding possible dose adjustment.
- In case of fever and suspicion of infectious diseases follow your national advice for access to health care and to test for Covid-19. In the meantime, withhold MTX and, if taking biologics, get in touch with your treating rheumatologist for guidance.”
Click here for the full statement.
Click here for translations in multiple languages.
From Rheumatologist Dr. Jack Cush at RheumNow
“First, it is important to counsel patients to NOT stop their anti-rheumatic, analgesic, anti-inflammatory, DMARD or biologic therapies. These are given to manage symptoms and/or to reverse inflammation or immune dysregulation. The message should be that uncontrolled disease is a much greater risk (because it would promote inflammation and immunosuppression) than the therapies we prescribe.”
AMRI: Associazione per le Malattie Reumatiche Infantili
COVID information for pediatric rheumatology patients (In Italian, but there is helpful info for anyone):
“….based on information currently available on the new coronavirus, children with rheumatic diseases are not at greater risk of infection…There is also no indication to discontinue immunomodulatory or immunosuppressive therapies except in special cases”
Click here for the complete letter in Italian.
Click here for the Google Translate link to English
FAI2R Flyer for COVID19
Click here for flyer in French
Click here for Google Translation in English
Arthritis Foundation Corona and Arthritis: What You Need to Know
“The CDC website goes on to say: “If you are at increased risk for
COVID-19 complications due to age or because you have a severe underlying medical condition, it is especially important for you to take actions to reduce your risk of exposure.” It recommends, if COVID-19 is spreading in your community, taking extra measures to put distance between yourself and other people, including staying home as much as possible and avoiding crowds, especially in poorly ventilated spaces.
We asked Michael George, MD, a rheumatologist and epidemiologist who studies infections in patients with autoimmune disease, who should follow this new guidance. He says. “The more at risk you are, the more you should consider this recommendation.”
He says this new guidance particularly applies to those with more severe
disease or who have been hospitalized in the past with a respiratory infection or have interstitial lung disease, COPD or asthma, for example. Those with more mild disease may want to ask their doctor for guidance.”
Click here for more from the Arthritis Foundation
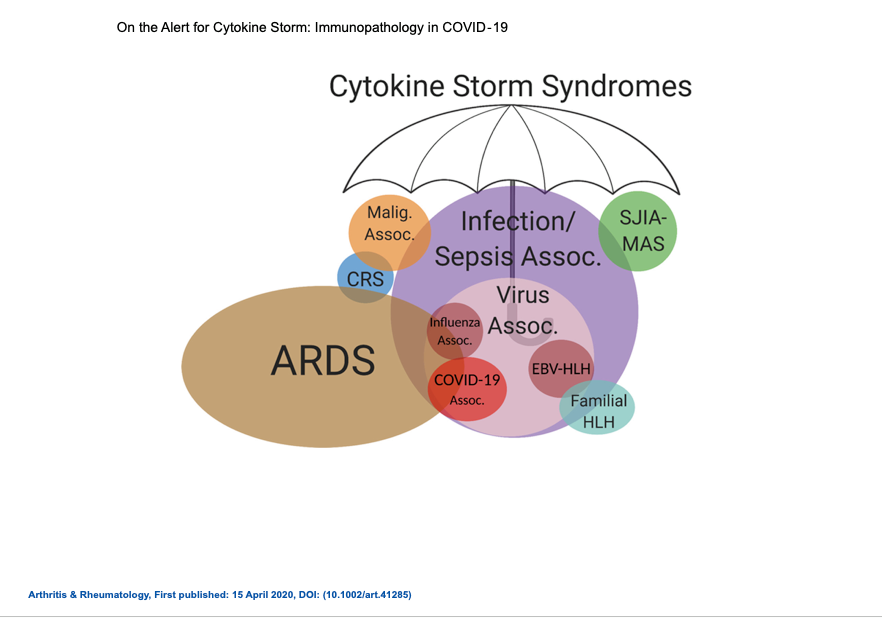
Multisystem Inflammatory Syndrome (MIS-C), COVID-19, and Autoinflammatory Diseases in Children
Information on MIS-C, the hyperinflammation syndrome that is affecting children possibly post COVID-19 infection, and autoinflammatory diseases.
CDC Coronavirus Disease 2019 (COVID-19) Page for High Risk Patients
https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications.html
World Health Organization (WHO) Q&A on coronaviruses (COVID-19)
here
https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
IPOPI Primary Immunodeficiency Statement
“There is currently no data pointing to whether PID patients are actually at
higher risk of more severe diseasefrom COVID-19(as per the WHO, CDCs and PID expert healthcare professionals and NMO representatives along with patients themselves).
However, it is believed that PID patients might be at higher risk for this
infection or a more severe course of the disease. Thus, patients with PID need to take extra care to prevent from getting this infection”
Click here for the full statement.
Primary Immune Foundation
Regularly updated page with current information. Click here.